百时美再受挫!NICE拒绝Opdivo用于肾癌治疗
2016-07-07 佚名 生物谷
百时美施贵宝的PD-1抑制剂Opdivo近年来一直在欧美监管方面所向披靡,迄今为止已经在美国斩获了非小细胞肺癌、肾细胞癌、黑色素瘤、经典霍奇金淋巴瘤等适应症,就在不久前还在晚期膀胱癌中收获了第六个突破性药物资格。然而,这一系列傲人战绩却在面对英国NICE时戛然而止。近日,NICE拒绝批准Opdivo用于治疗肾癌。百时美对NICE的这一决定表示非常不满,然而NICE的指南草案却认为,目前没有充分的试

百时美施贵宝的PD-1抑制剂Opdivo近年来一直在欧美监管方面所向披靡,迄今为止已经在美国斩获了非小细胞肺癌、肾细胞癌、黑色素瘤、经典霍奇金淋巴瘤等适应症,就在不久前还在晚期膀胱癌中收获了第六个突破性药物资格。然而,这一系列傲人战绩却在面对英国NICE时戛然而止。近日,NICE拒绝批准Opdivo用于治疗肾癌。
百时美对NICE的这一决定表示非常不满,然而NICE的指南草案却认为,目前没有充分的试验数据表明Opdivo治疗晚期肾细胞癌患者的长期获益情况。此外,NICE的药物评估委员会表示,使用Opdivo后患者每个质量调整生命年的增量成本效果比超过了6万英镑,这对于医保无疑是非常沉重的负担。
百时美对NICE的这一决策表示遗憾,尽管临床数据已经证明Opdivo能够延长晚期肾细胞癌患者的整体生存期,但是NICE将其拒之门外,意味着英国的患者无法通过NHS获得Opdivo的有效治疗。
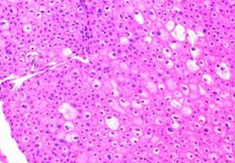
目前Opdivo已经被NICE批准用于治疗晚期黑色素瘤,但是非小细胞肺癌和肾细胞癌却不在适应症范围之内。肾细胞癌患者中,约27%在确诊时就已经是晚期,其预后较差,治疗的首要目的就是延长患者的生存时间。
百时美表示,Nivolumab已经在多个适应症中获得了欧美监管机构的一致肯定,百时美一直致力于通过一切可能的办法让NHS的患者得到该药物的有效治疗。百时美曾通过英国的早期获药计划(EAMS)让388名不同类型的癌症患者使用了Nivolumab,现在希望英国的药物成本监管机构NICE能够本着对患者负责的态度,批准该药物治疗肾细胞癌。
有试验结果表明,和诺华的mTOR抑制剂Afinitor (everolimus)相比,Nivolumab治疗肾细胞癌患者的生存期显着延长了5.6个月(25个月VS19.6个月)。据悉接下来还有四周的上诉和回应时间,最终决定将在四周后公布。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#百时美#
40
NICE还是比较务实
94
#NICE#
40
#Opdivo#
42