Int J Cancer:新辅助系统疗法对胃肠道间质瘤预后的影响
2021-03-02 MedSci原创 MedSci原创
予以局限性GIST患者新辅助系统疗法与适度的生存益处和较低的术后90天死亡率相关,且不影响R0切除的可能性。
回顾性和单臂前瞻性研究已经报道,使用新辅助药物伊马替尼治疗胃肠道间质瘤(GIST)可获得一定临床益处。但目前还没有相关的随机III期研究数据,因此,新辅助系统疗法(NAT)与早期切除术(UR)相比对生存率的影响仍不清楚。
本研究旨在对比新辅助系统疗法与早期切除术相比对GIST患者预后的影响。
研究人员从国家癌症数据库(2004年-2016年)中筛选了16308名接受了胃、食管、小肠和结肠的局限性GIST切除术的患者,他们还进行了或未进行3个月及以上的NAT治疗。采用加权的时间依赖性Cox比例风险模型估计了NAT对总生存率的影响,并用加权Logistic回归分析了NAT对术后90天死亡率和根治(R0)切除术的影响。
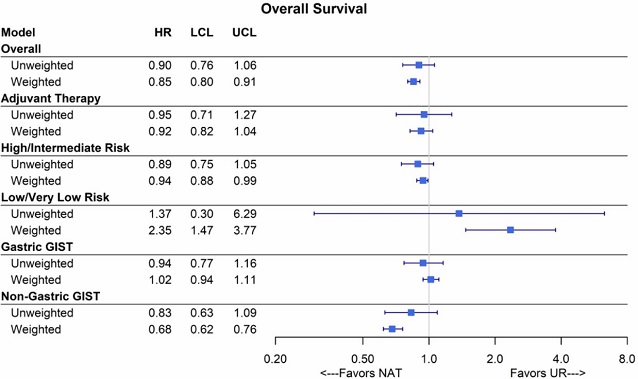
两组的总存活率
865名(5.3%)患者接受了NAT治疗,15443名(94.7%)患者接受了UR治疗。中位NAT持续时间为6.3个月。NAT组和UR组的男性患者占比分别为53.7%和48.6%,原发性GIST的患者占比分别为67.3%和65.1%,高风险患者占比分别为72.8%和49.7%。
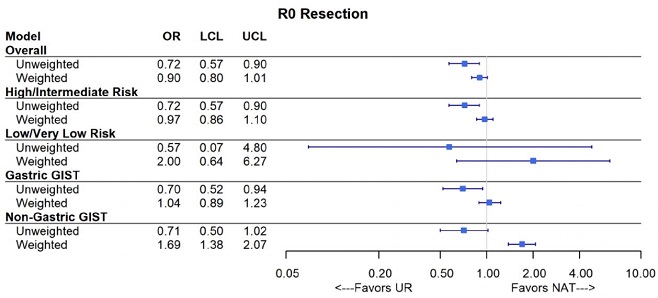
两组的R0切除率
NAT组患者的肿瘤体积较大,核分裂指数较高。接受NAT治疗超过3个月与显著的生存益处相关(加权HR 0.85[0.80~0.91])。NAT组患者术后90天死亡率为4/865(0.5%),而非NAT组患者的为346/15443(2.2%)。NAT与较低的术后90天死亡率相关。不同组间的R0切除率无明显差异。
总而言之,虽然NAT患者的风险较高,但这项分析表明,予以局限性GIST患者新辅助系统疗法与适度的生存益处和较低的术后90天死亡率相关,且不影响R0切除的可能性。
原始出处:
Marqueen Kathryn E,Moshier Erin,Buckstein Michael et al. Neoadjuvant therapy for gastrointestinal stromal tumors: A propensity score weighted analysis. Int J Cancer, 2021, 10.1002/ijc.33536
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新辅助#
52
学习
91
#胃肠道#
42
#间质瘤#
64
进来看看新内容,新知识
98