Blood:与多发性骨髓瘤来那度胺或泊马度胺获得性耐药相关的CBRN变异
2020-08-11 MedSci原创 MedSci原创
约1/3的骨髓瘤患者对泊马度胺耐药时会出现CBRN变异;CBRN变异与来那度胺难治性骨髓瘤患者采用泊马度胺治疗时的预后差相关。
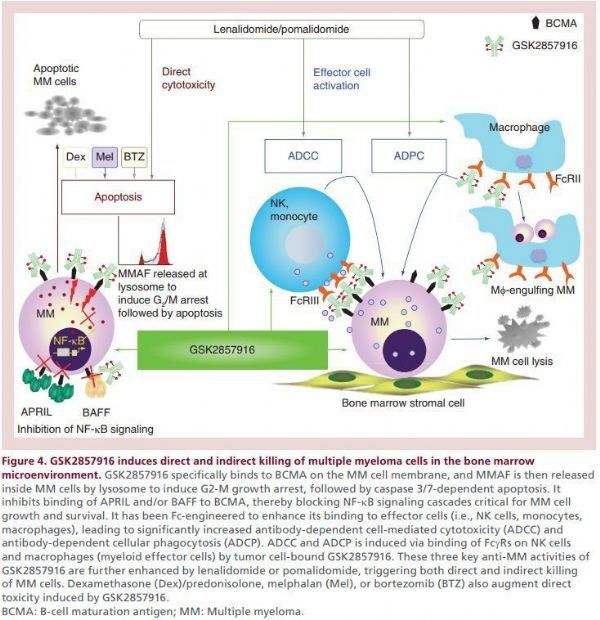
对所有可用治疗的耐药性的出现是提高骨髓瘤患者存活率的主要挑战。Cereblon (CRBN)是骨髓瘤中广泛使用的IMiD和新型CelMOD药物以及正在开发用于多种疾病的某些PROTAC的必需结合蛋白。
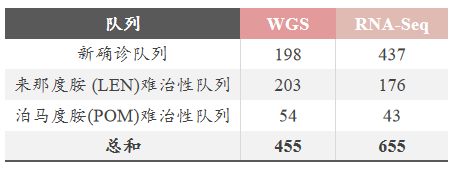
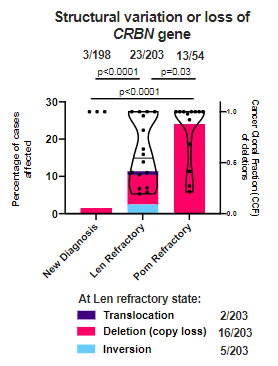
利用455位患者的全基因组测序数据和655位患者的RNA测序数据,研究人员发现三种CRBN变异(即点突变、拷贝数缺失/结构变异和特殊转录本变异[如外显子10剪切变异])的发生频率逐渐增加,伴随IMiD进行性暴露,直到约1/3的进展为POM难治性的患者出现CBRN变异。
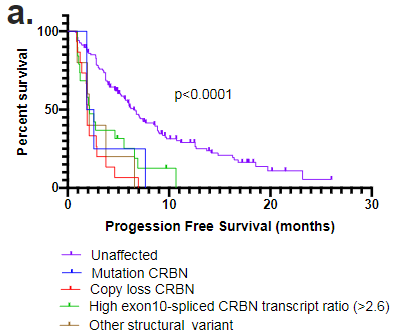
研究人员发现,这三种CRBN变异均与LEN难治性患者采用POM治疗效果差相关,包括既往未研究过的携带拷贝数缺失和结构变异的个体。
据了解,本研究是首次对治疗中进展的骨髓瘤患者CBRN变异进行综合分析的研究,有助于指导患者选择CRBN靶向药物的序贯疗法。
原始出处:
Sarah Gooding,et al. Multiple Cereblon genetic changes associate with acquired resistance to Lenalidomide or Pomalidomide in Multiple Myeloma. Blood. August 4,2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#获得性#
39
#获得性耐药#
43
#CBR#
27
谢谢
83
#变异#
34
#多发性#
0
谢谢
93