JAHA:肾功能和房颤之间的双向关联
2022-05-18 MedSci原创 MedSci原创
肾功能,尤其是eGFRcys,与房颤之间存在双向相关性。目前还没有针对轻度慢性肾病患者的房颤的预防措施,反之亦然。该研究的结果为改善这两种疾病的预测/预防提供了初步依据。
心房颤动和慢性肾脏疾病是非常常见的疾病。更具体地说,全世界每年约有500万新发房颤病例,而全球约11%至13%的人群伴有慢性肾脏病。此外,这两种疾病都与大量的心脑血管疾病发病率和死亡率有关。但目前关于肾脏功能与房颤之间的双向关联缺乏一致的认识,这对于慢性肾脏疾病和房颤的预防/治疗都是至关重要的信息。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,因此,研究人员旨在明确肾功能与房颤之间的双向关联。
该研究为前瞻性队列研究,研究人员纳入了9228名参与者(平均年龄为64.9岁;57.2%为女性),他们具有肾功能(根据血清肌酐[eGFRcreat]、胱抑素C[eGFRcys]或尿白蛋白-肌酐两者[eGFRcreat-cys]比值估计肾小球滤过率[eGFR])和房颤的信息。肾功能降低被定义为eGFRcreat<60ml/min/1.73m2。研究人员采用Cox比例风险、logistic回归、线性混合和联合模型来探究肾功能与房颤之间的关系,反之亦然。
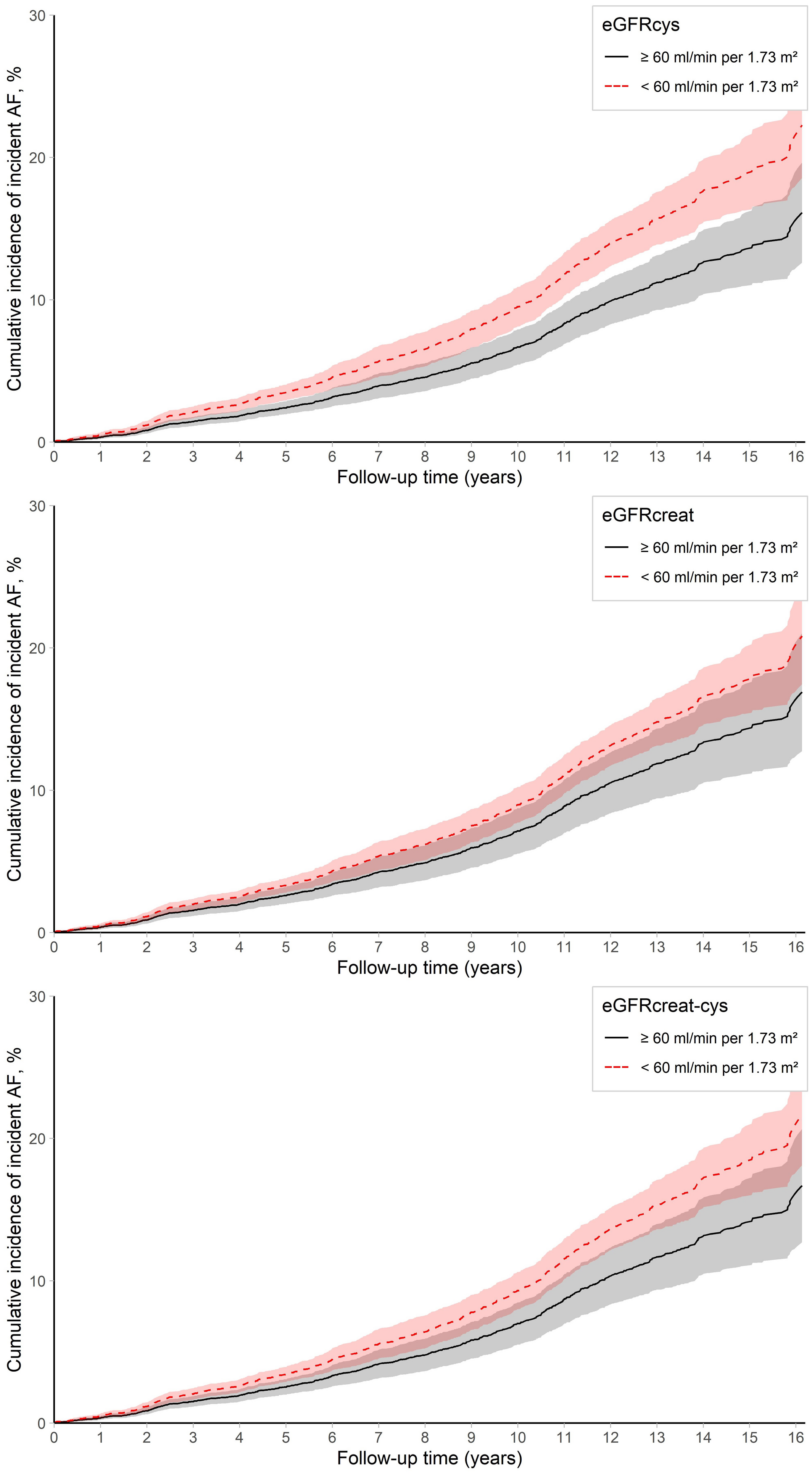
在随访期间(中位时间为8.0年),研究人员共记录到了780起房颤事件。较低的eGFRcys和eGFRcreat-cys与房颤风险增加相关(eGFR每降低10mL/min/1.73m2,风险比为1.08[95%CI为1.03-1.14],风险比为1.07[95%CI为1.01-1.14])。对于eGFRcys和eGFRcreat-cys,房颤的10年累积发生率分别为16%(eGFR<60)和6%(eGFR≥60)。伴有房颤(与不伴有房颤相比)与eGFRcreat降低2.85mL/min/1.73m2相关,且也与随着年龄增长的更快的eGFRcreat下降速度有关。伴有房颤与肾功能下降的风险增加1.3倍相关。
由此可见,肾功能,尤其是eGFRcys,与房颤之间存在双向相关性。目前还没有针对轻度慢性肾病患者的房颤的预防措施,反之亦然。该研究的结果为改善这两种疾病的预测/预防提供了初步依据。
原始出处:
Anna C. van der Burgh.et al.Bidirectional Association Between Kidney Function and Atrial Fibrillation: A Population‐Based Cohort Study.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.122.025303
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习了
41
#肾功能#
48
原来如此
42
学习了
52
#AHA#
0
学习了,很好
41
签到学习
50