弹性钉联合带线锚钉治疗成人桡骨颈骨折伴肘关节脱位1例
2019-07-17 高旭 尹海磊 卢建峰 临床骨科杂志
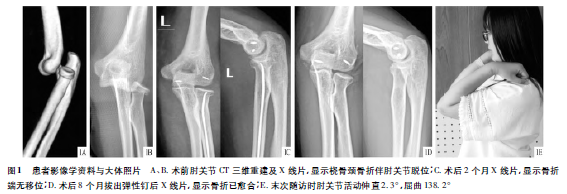
患者,女,20岁,玩滑板时不慎摔倒,伤后5h入院。查体:肘部肿胀,有压痛,患侧肘关节伸直屈曲活动受限。入院后肘关节CT三维重建及X线检查显示桡骨颈骨折伴肘关节脱位(见图1A、B)。臂丛麻醉下手术。
临床资料
患者,女,20岁,玩滑板时不慎摔倒,伤后5h入院。查体:肘部肿胀,有压痛,患侧肘关节伸直屈曲活动受限。入院后肘关节CT三维重建及X线检查显示桡骨颈骨折伴肘关节脱位(见图1A、B)。臂丛麻醉下手术。
患者仰卧位,患肢外展,行Kocher手术入路。术中探查见外侧副韧带断裂,于肱骨外髁中心置入2.7mm带线锚钉修复外侧副韧带(未切开环装韧带),C臂机透视见肘关节复位不满意。于肘关节后内侧入路行小切口,长约6CM,探查见内侧副韧带部分撕裂,于肱骨内髁置入2.7mm带线锚钉加强缝合撕裂韧带。再次透视见肘关节复位满意,冲洗切口,逐层缝合。于桡骨茎突近端2CM处做纵向切口,长约2CM,注意避免损伤桡神经浅支。牵拉开伸肌腱并切开骨膜,钛质弹性钉直径选用髓腔最小直径的60%,对弹性钉尖端下方进行预弯,预弯的顶点尽量靠在桡骨粗隆附近。由助手固定肘关节外展,开口器在桡骨外侧开口,将弹性钉穿入髓腔,尖端朝向前外侧,弹性钉尖端与骨折块接触后,敲击尾端使弹性钉尖端嵌入桡骨小头关节面下方的松质骨,在C臂机透视下多次敲击钉尾直至骨折复位。
复位后透视见位置好,最后轻敲尾端使尖端与松质骨衔接稳固,保留钉尾0.5CM的长度置于皮下。术后2周拆线,患肢功能位石膏外固定3周。拆除石膏后,逐步进行肘关节屈伸功能锻炼。术后2个月复查,骨折端对位对线位置可,未发生骨折移位(见图1C)。术后8个月拔出弹性钉,骨折已愈合,骨折线消失(见图1D)。术后随访24个月,未出现感染、骨不愈合或畸形愈合、桡骨头坏死等并发症。末次随访时测量屈肘、伸肘度数分别为138.2°、2.3°(见图1E),前臂旋转活动度与对侧基本一致,Mayo肘关节评分为95分。
原始出处:
高旭,尹海磊,卢建峰.弹性钉联合带线锚钉治疗成人桡骨颈骨折伴肘关节脱位1例[J].临床骨科杂志,2019,22(03):330+333.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#带线锚钉#
35
#关节脱位#
34
#肘关节脱位#
43
#肘关节#
38
#脱位#
41
#桡骨#
31