JAMA子刊:儿童心脏病死亡后家属的临终关怀有多难?
2022-05-08 liangying 网络
在缺乏儿科心脏重症监护病房(CICUs)临终关怀质量指标的情况下,跨学科工作人员如何看待死亡质量(QODD)?
尽管医学和外科技术取得了进步,但先天性和后天性心脏病仍然是儿童死亡的主要原因。儿童心脏病死亡在心脏重症监护病房(CICU)发生率很高,在复杂的CICU环境中为儿童及其家人提供临终关怀尤其具有挑战性。儿童死亡违反了自然的代际循环,给相关家庭带来了巨大的悲痛,这些复杂性会导致冲突产生,家属的态度可能会对员工产生负面影响,并导致道德伤害。
心脏重症监护病房(CICU)的跨学科工作人员发挥着不可或缺的作用,为儿童和临终家庭提供支持。本研究的目的在于评估儿科重症监护病房死亡质量(PICU-QODD)仪器,并探讨不同学科和临终环境之间的差异。
这项横断面调查纳入2019年7月1日至2021 6月30日期间一个中心的儿童CICU死亡人员。
结果显示,在60例死亡儿童中,33例(55%)接受了重症监护。共进行了713项调查(72%的回复率),其中246项(35%)来自护士,208项(29%)来自医生,259项(36%)来自专职医疗人员。临床经验各不相同。PICU-QODD评分中位数(IQR)为93(84-97),死亡瞬间质量评分和7天前评分分别为9分(7-10分)和5分(2-7分)。Cronbachα的范围为0.87(医务人员)到0.92(联合健康),PICU-QODD分数与全球评分和校准问题显著相关。护理人员和专职医疗人员的PICU-QODD平均分(SD)比执业医师低3分以上(护理人员:88.3[10.6];专职医疗人员:88.9[9.6];执业医师:91.9[7.8];P<0.001)。
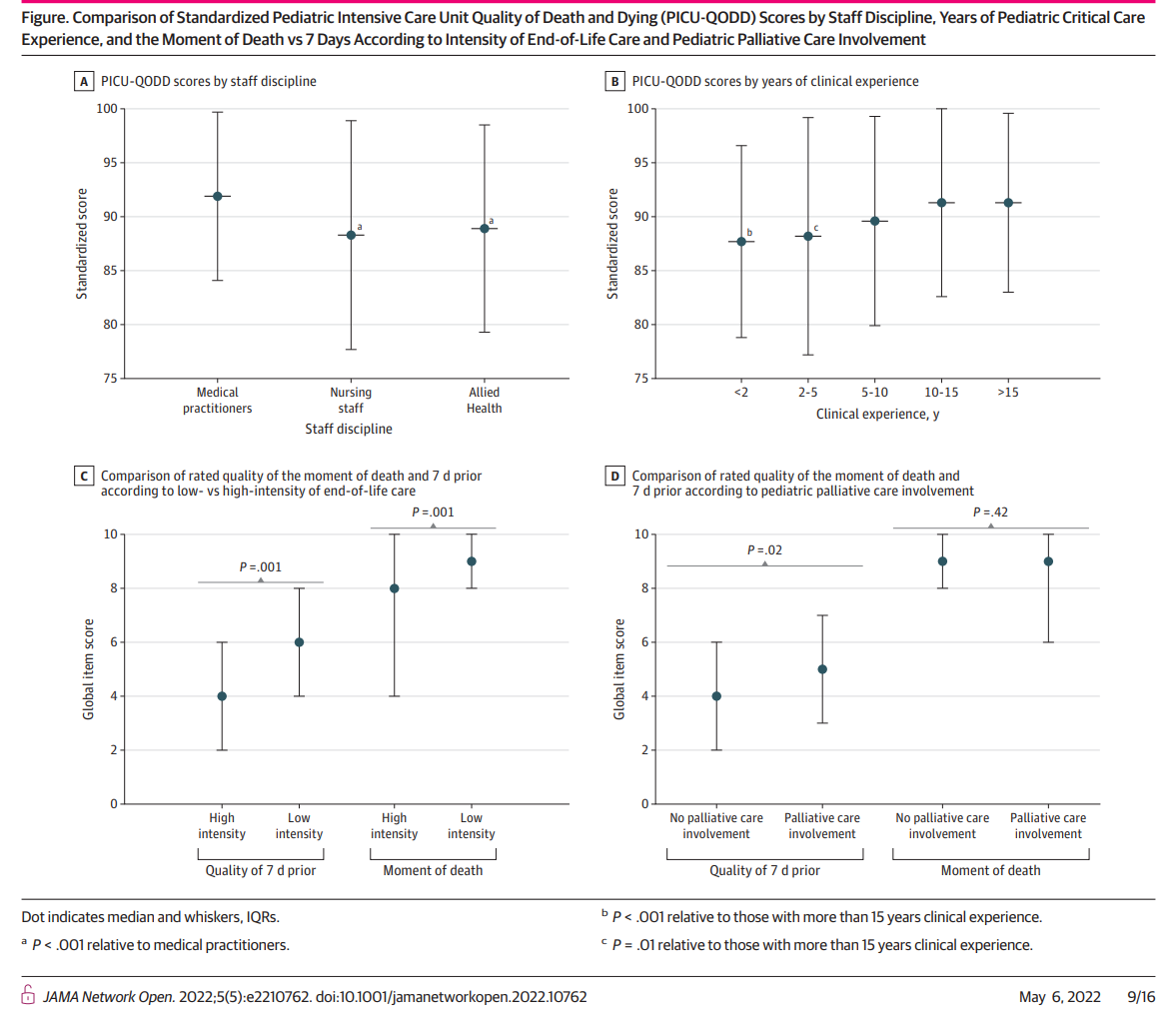
根据临终关怀强度和儿科姑息治疗参与程度,儿科重症监护标准化病房死亡和死亡质量(PICU-QODD)评分
患有合并症、因手术入院、治疗后死亡或死亡与家人意愿不符的患儿的平均PICU-QODD评分较低。姑息治疗的参与没有观察到差异。与低强度护理相比,高强度护理与死亡前7天(4[2-6]vs 6[4-8];P=0.001)和死亡时刻(8[4-10]vs 9[8-10];P=0.001)的质量中位数(IQR)较低有关。
总之,在这项针对CICU工作人员的横断面调查研究中,PICU-QODD有望成为衡量CICU死亡质量的可靠有效的临床医生指标。总体来说QODD被认为是积极的,死亡前7天的评分质量较低,员工和患者特征也存在差异。这些数据可以帮助改善CICU工作人员的福祉以及患者和家属的临终体验的策略。
参考文献:
Bailey V, Beke DM, Snaman JM, et al. Assessment of an Instrument to Measure Interdisciplinary Staff Perceptions of Quality of Dying and Death in a Pediatric Cardiac Intensive Care Unit. JAMA Netw Open. 2022;5(5):e2210762. doi:10.1001/jamanetworkopen.2022.10762
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#心脏病死亡#
42
#临终关怀#
48
#临终#
39
#儿童心脏病#
42
JAMA上文章都是顶级的,谢谢梅斯及时上新
33