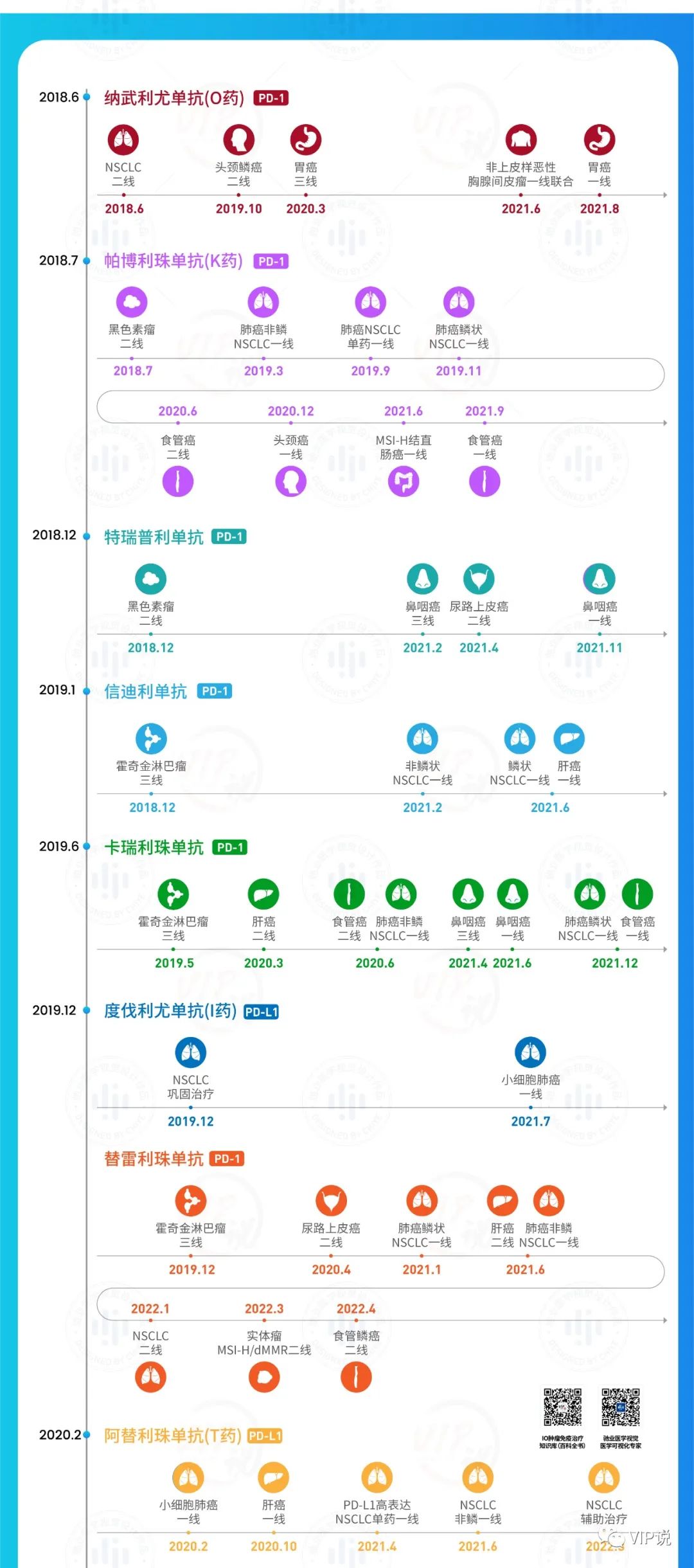
2021年发布的《一图读懂中国PD-1/PD-L1治疗发展史》,受很多读者喜欢,时隔4个月后横空出世重制版,更新日期截至2022.4.28,让您捋顺中国PD-1/PD-L1格局,附精彩点评和高清长图下载链接!


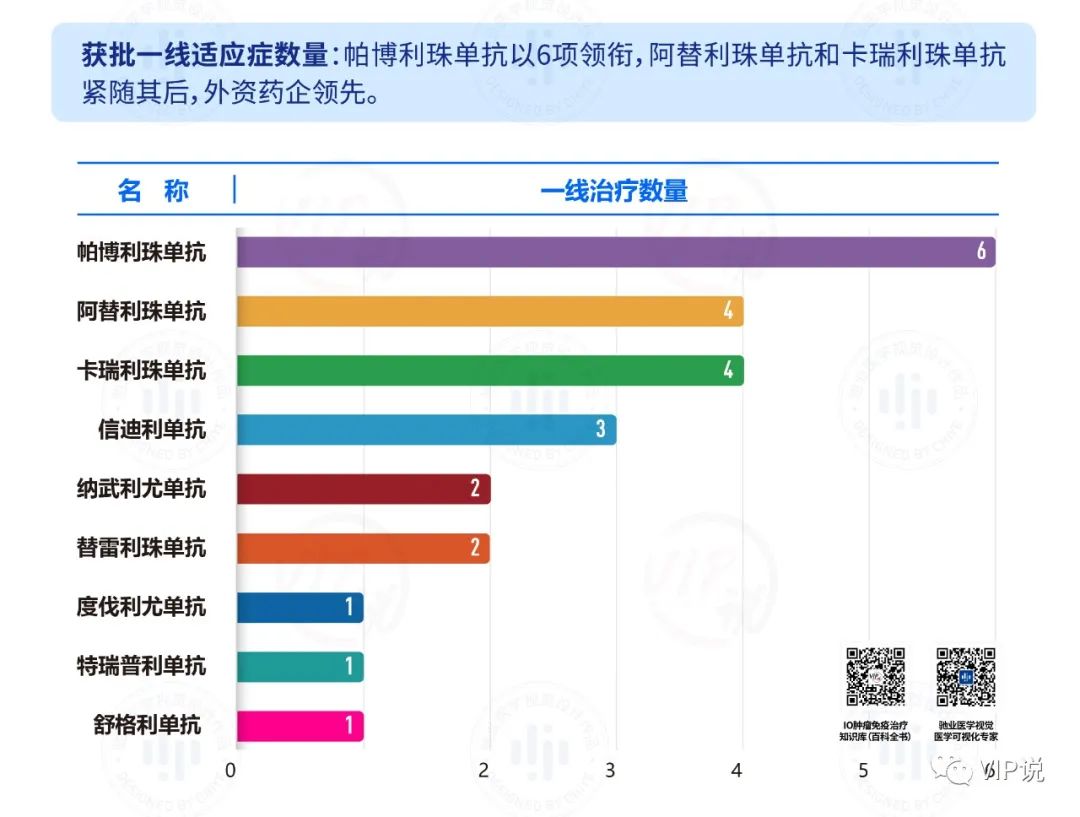

一线适应症
一线适应症涉及9个癌肿,分别是:
1、非小细胞肺癌:共5款PDX获批晚期一线(鳞癌和非鳞)治疗,分别是
-
PD-1 4款 (K药、替雷利珠单抗、卡瑞利珠单抗、信迪利单抗)
-
PD-L1 1款(舒格利单抗)
-
T药虽仅获批NSCLC非鳞一线,但独拥NSCLC辅助治疗适应症,而I药则独拥NSCLC巩固治疗,独孤求败!
2、小细胞肺癌:共2款(PD-L1:T药、I药),尽是进口PD-L1的天下,但国产的PD-1斯鲁利单抗注册三期达到终点,期望年内获批。
3、肝癌:共2款(T药和信迪利单抗),一线联合方案霸屏,Ibrave150的优效头对头研究可以吹嘘好一阵了,但肝癌今年最震撼的估计是君实辅助治疗数据的读出。
4、食管鳞癌:共2款(K药和卡瑞利珠单抗),其余三小强虎视眈眈,就在27日百济的食管癌一线研究也达到主要终点,不用想,又是新一波内卷的开始。
5、胃或胃食管连接部腺癌:共1款(O药),这里需要表扬下信达,国产里唯一率先达到终点的PD-1,打破垄断在即。
6、头颈鳞癌:共1款(K药),似乎国产PDX没什么布局。
7、结直肠癌:共1款(K药),其实是借助了MSI-H的东风,希望未来去掉Biomarker,踏踏实实的攻破结直肠癌。
8、鼻咽癌:共2款(特瑞普利单抗、卡瑞利珠单抗),广东癌,中国癌中国治,仅有国产PD-1在列,百济的三期数据也紧随其后。
9、非上皮样恶性胸膜间皮瘤:共1款(O药),no comments
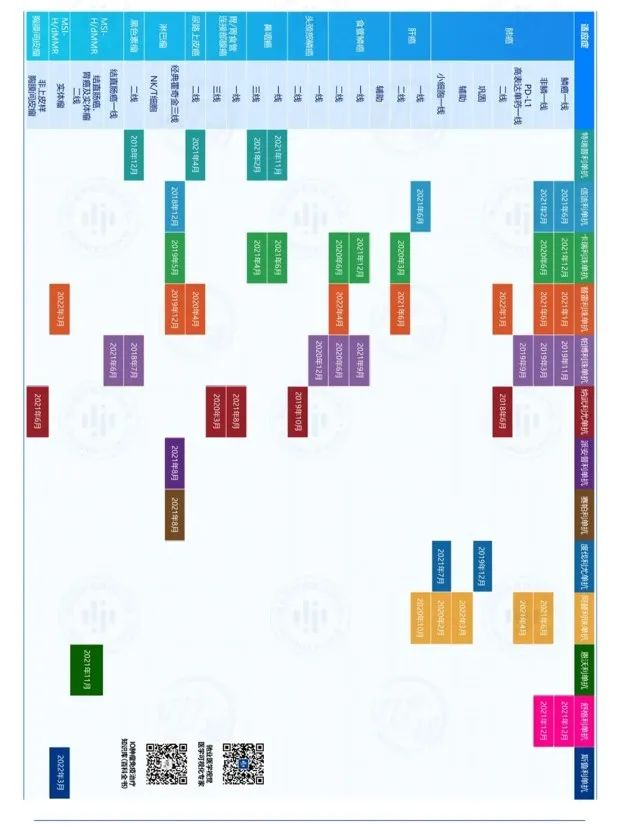
二线及以后适应症
不做详细点评了,个别拎出来说一说:
1、非小细胞肺癌、肝癌、食管癌、胃癌:大癌种一线都快玩烂了,不要再跑后线了,赶紧往前跑吧,什么辅助新辅助的。
2、鼻咽癌:不出意外三个国产PD-1占领这个领域,癌种不大,就别扎堆了,这三家玩三国就好了。
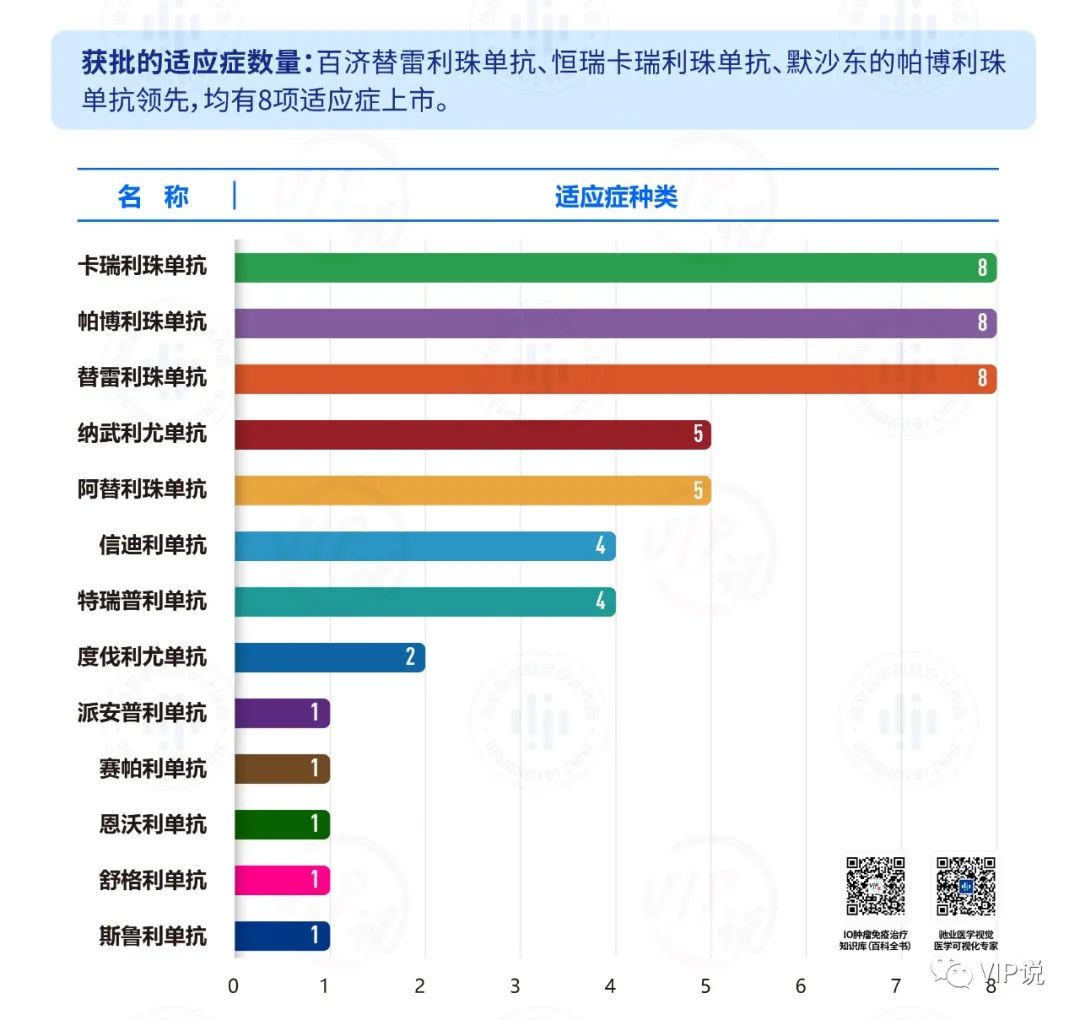
3、霍奇金淋巴瘤:批了5款,打桌麻将都富余一个,国内都13种PDX了,估计后续无法再靠这个小癌种获批上市了。
4、黑色素瘤:国产进口各一款,二线都批了快四年了,两位大佬赶紧往一线走啊,人群少也需要药的。
5、尿路上皮癌:国人似乎对于泌尿系肿瘤不感冒,就两款国产PD1画了个楚汉边界,目前就看谁的一线首先进咸阳。
6、MSI-H/dMMR 实体瘤:共3款,也是个走捷径的绿色通道,目前还能斗地主,三缺一,后续别再以这种适应症上市了。
2022年新增适应症
22年到现在都快5个月了,就斯鲁利单抗一个产品获批,适应症也就批了5个。
看样子经过了2021年PDX的内卷高光时刻后,上市速度也乏力了,就目前在申请适应症看,下半年将是另一高潮的到来,都是大适应症啊。
1、斯鲁利单抗:2022年3月MSI-H/dMMR实体瘤适应症
2、替雷利珠单抗3个二线适应症:
-
2022年1月NSCLC二线
-
2022年3月MSI-H/dMMR实体瘤2线
-
2022年4月食管鳞癌二线
3、T药:2022年3月NSCLC辅助治疗适应症(高光啊)
PS:高清原版全图,请在肿瘤新前沿公众号,后台回复“0428“即可。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











总结走心,期待更新!
62
感谢
47
0428
44
#PD-L1#
44
感谢分享
62
***
58