JAHA:美国心源性休克患者住院率和院内死亡率的趋势
2021-07-28 MedSci原创 MedSci原创
在2004年1月至2018年12月期间,归因于CS的住院人数增加了两倍。然而,在研究期间,CS住院死亡率缓慢下降。需要进一步的研究来确定最近采用的治疗是否会进一步影响CS患者的院内死亡率。
目前,缺乏关于心源性休克(CS)患者院内死亡率趋势的当代数据。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员从美国国家住院患者样本中确定了2004年1月1日至2018年12月31日入院的CS患者。研究人员报告了总体人群和选定亚组中院内死亡率的原始和调整趋势。

在2004年1月1日至2018年12月30日期间,总共563949644例住院治疗患者,其中1254358例(0.2%)患者死亡归因于CS。归因于CS的住院人数稳步增加,从2004年的每10万住院患者中122人增加到2018年每10万住院患者中408人(趋势P<0.001)。
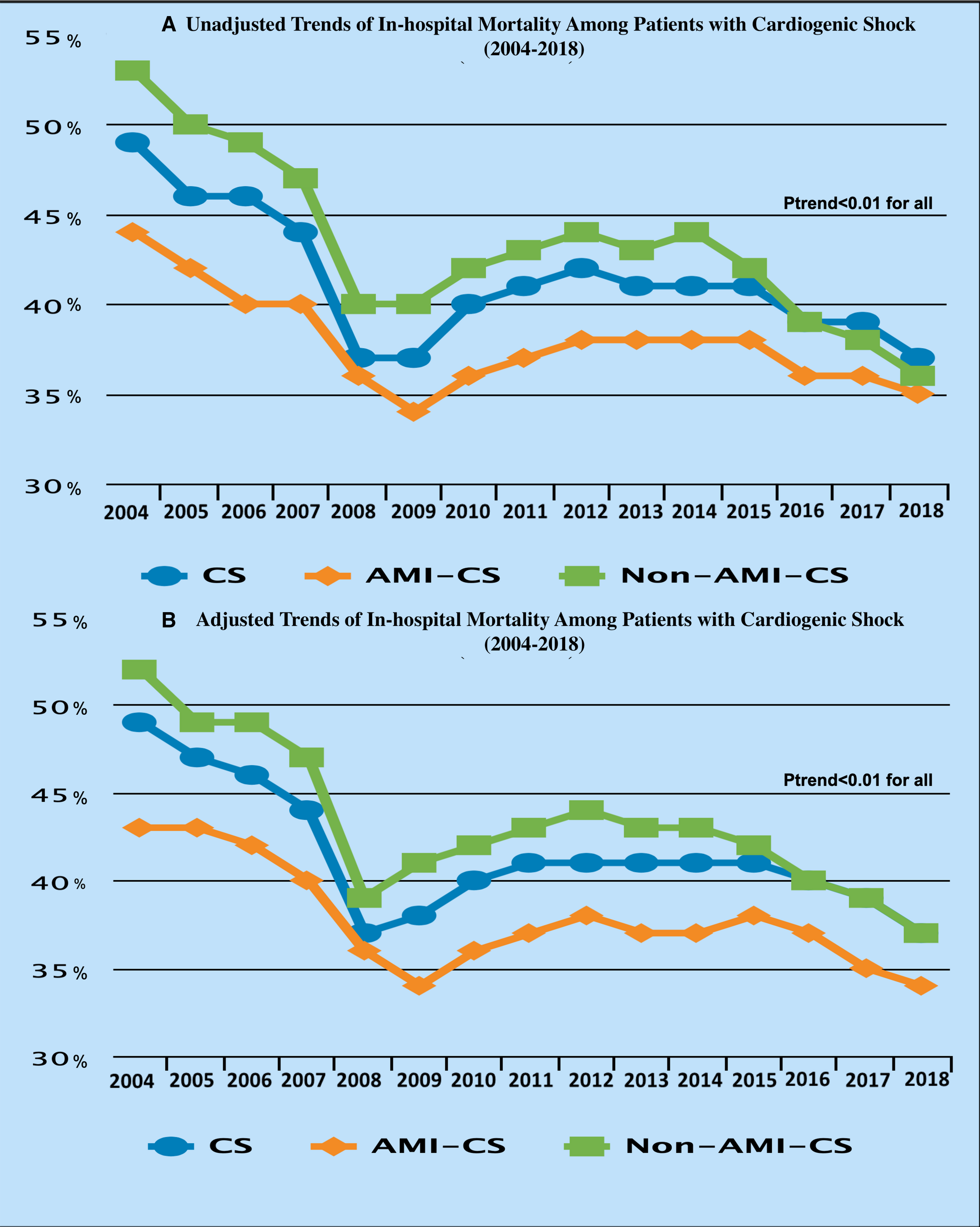
研究期间CS患者住院死亡率趋势
这些结果与研究期间整体人群(从2004年的49%到2018年的37%;趋势P<0.001)、急性心肌梗死的CS患者(从2004年的43%到2018年的34%;趋势P<0.001)以及非急性心肌梗死CS患者(从2004年的52%到2018年的37%;趋势P<0.001)的住院死亡率调整趋势稳步下降相关。无论医院教学状况如何,女性、男性、不同种族/族裔群体、不同地区和不同医院规模都存在死亡率降低的一致性趋势。
由此可见,在2004年1月至2018年12月期间,归因于CS的住院人数增加了两倍。然而,在研究期间,CS住院死亡率缓慢下降。需要进一步的研究来确定最近采用的治疗是否会进一步影响CS患者的院内死亡率。
原始出处:
Mohammed Osman.et al.Fifteen‐Year Trends in Incidence of Cardiogenic Shock Hospitalization and In‐Hospital Mortality in the United States.JAHA.2021.https://www.ahajournals.org/doi/10.1161/JAHA.121.021061
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#院内死亡#
33
#AHA#
38
#心源性休克#
41
#心源性#
30
这些数据很真实
64