PAH与PH-HFpEF如何区别
2022-05-19 刘少飞 MedSci原创
鉴于其对PAH治疗的积极反应,PH在HFpEF中的作用目前正受到密切关注,因为它约占HF患者的50%,对流行病学影响很大,而且缺乏有效管理。
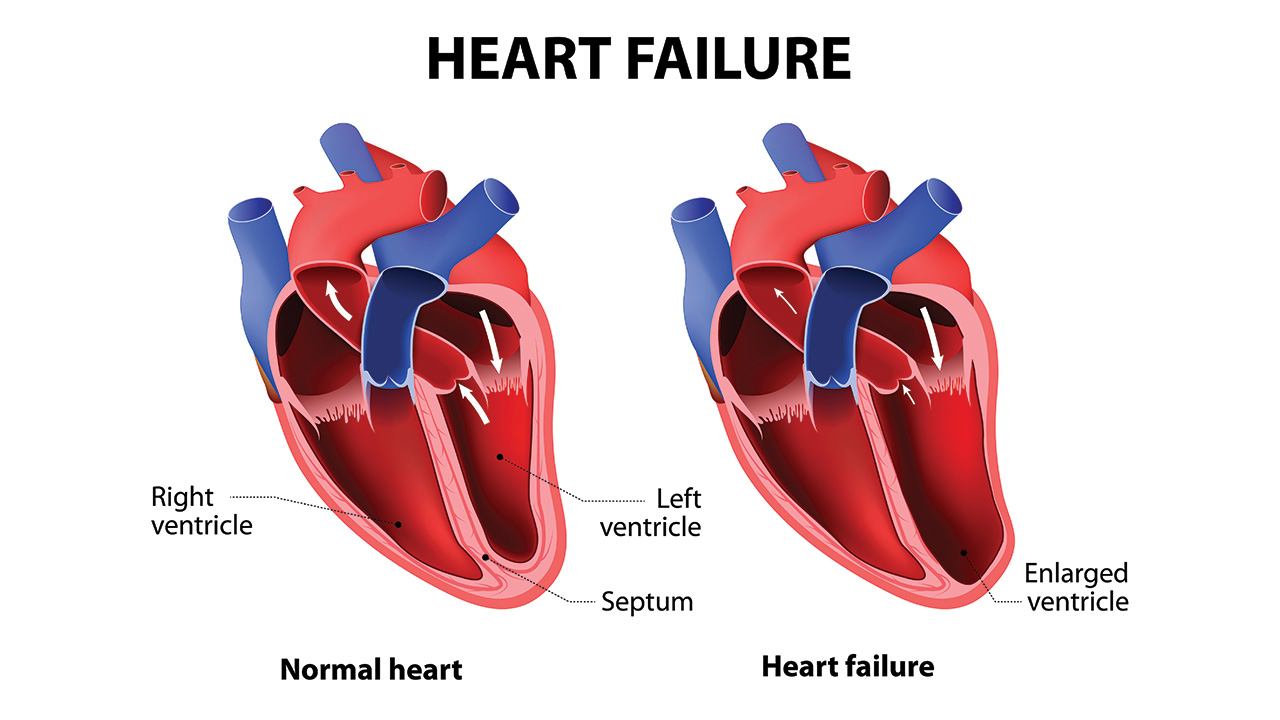
在射血分数保留的心力衰竭的背景下,越来越多的证据表明PH-HFpEF的晚期阶段与PAH表型的晚期阶段有重合。大多数PH-HFpEF患者有孤立的毛细血管后PH(IpcPH),持续的PAWP升高导致肺静脉血管重塑,但不引起PVR增加,PVR保持在≤3WU。因此,PH-LHD患者的典型血流动力学特征是PAPm没有过度升高(25-40mmHg),由PAWP升高(通常>20mmHg),心脏指数低,经肺梯度升高(TPG>12mmHg),或右心房压力持续升高(>10mmHg)。相反,在LA压力正常的情况下,PAH疾病的定义是静息时PAPm≥25 mmHg,肺动脉楔压(PAWP)≤15 mmHg,肺血管阻力(PVR)>3伍德单位(WU)。此外,PAH的疾病过程似乎主要位于动脉血管,没有静脉的参与。当PH-HFpEF进展时,病理开始影响远端肺动脉,导致PH的毛细血管前成分的发展,即PVR升高(>3WU),以及合并毛细血管前和后PH(CpcPH)。
鉴别PH-HFpEF中的毛细血管前成分至关重要,因为与IpcPH相比,CpcPH的预后要差得多,运动能力下降,管理方式不同,对PAH特异性血管舒张剂的反应也不同。一项对2587名患者的回顾性分析证明,CpcHF的标志物,如DPG≥12mmHg,TPG≥12mmHg,PVR≥3WU,是死亡和心衰住院的预测因素。
第5届WSPH提出了3个步骤的方法,以帮助区分第2组和PAH,使用测试前的概率评分来定义更有可能接受有创血流动力学定义的患者,并预测结果和预后。与PAH表型相比,PH-HFpEF具有特殊的人口学、临床和超声心动图特征,包括年龄大、女性、高血压、心房颤动率高、代谢综合征(高脂血症、肥胖、糖尿病和高血压)。
到目前为止,已经提出了许多评分标准,整合了回顾性单中心研究分析的特征;有些人甚至认为,仅有简单的临床特征,没有超声心动图或血流动力学数据,就能区分PH-HFpEF与PAH。到目前为止,还没有一个评分得到外部验证,但最近有人提出了一个类似的方法来评估慢性心衰患者的HFpEF。对CpcPH-HFpEF和PAH表型的研究导致了对 "典型PAH"、"非典型PAH "和PH-HFpEF(CpcPH)患者的亚分类的确定。第二类包括年龄较大的PAH患者和心血管合并症的高负担(定义为存在至少三个左心室功能障碍的危险因素,包括上面列出的因素)。这些表型首先在AMBITION(安布生坦和他达拉非在肺动脉高压患者中的应用)试验中被确定,其中 "非典型PAH "患者被排除在主要分析集之外。对多国肺动脉高压新疗法比较、前瞻性登记(COMPERA)中的5935名患有PH并接受过至少一种PH靶向治疗的患者的分析表明,与 "典型 "PAH患者相比,CpcPH-HFpEF患者的效果不明显,而 "非典型 "类别则处于两者之间。这支持了从 "典型 "PAH和HFpEF合并PH有一个连续性的假设,但需要更多的研究来评估PAH治疗对CpcPH的影响,因为任务组仍然不推荐在任何类型的PH-LHD中使用它们。
参考文献:
Barilli M, Tavera MC, Valente S, Palazzuoli A. Structural and Hemodynamic Changes of the Right Ventricle in PH-HFpEF. Int J Mol Sci. 2022 Apr 20;23(9):4554. doi: 10.3390/ijms23094554. PMID: 35562945; PMCID: PMC9103781.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
36
精彩评论,需要您登录查看
52
#HFpEF#
59
#PAH#
46