Thyroid:左旋甲状腺素/ L-三碘甲状腺原氨酸与左旋甲状腺素单药治疗成人甲状腺功能减退患者的利弊的系统综述和荟萃分析
2021-10-22 从医路漫漫 MedSci原创
左旋甲状腺素(LT4)/ L-三碘甲状腺原氨酸(LT3)联合治疗作为LT4单药治疗的潜在替代疗法已引起临床医生和患者的关注。
背景:左旋甲状腺素(LT4)/ L-三碘甲状腺原氨酸(LT3)联合治疗作为LT4单药治疗的潜在替代疗法已引起临床医生和患者的关注。本研究的目的是比较LT4/LT3联合治疗和LT4单药治疗对甲状腺功能减退患者的益处和危害。
方法:由一名图书馆员从MEDLINE、Scopus、EMBASE、Web of Science和Cochrane Central Register of Controlled Trials开始系统检索,直到2020年9月。对成年甲状腺功能减退患者进行联合治疗(LT4/LT3)与单药治疗(LT4)的随机临床试验和准实验研究被考虑纳入研究。由评审员进行独立数据提取。对临床结果和患者偏好进行meta分析,比较每种治疗效果的标准化平均差异。以叙述方式评估不良事件和反应的比例。
结果:共检索到文献1398篇,符合纳入标准的文献18篇。结果支持的证据,在临床状态,生活质量,心理困扰,抑郁症状和疲劳方面,没有显示治疗效果的差异;所有这些都是通过标准化问卷测量的。此外,患者偏好的荟萃分析显示,与单药(23%)或无偏好(30%)相比,选择联合治疗的比例(43%)更高。评价治疗不良事件或不良反应时,治疗组间比例相近。

图1 偏差风险评估。
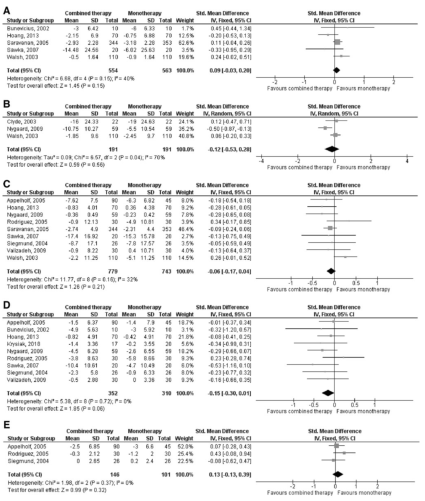
表 比较LT3/LT4联合疗法和LT4单一疗法在(A)临床状态、(B)生活质量、(C)心理困扰、(D)抑郁症状和(E)疲劳方面的疗效。LT3,L-三碘甲状腺原氨酸;LT4,左旋甲状腺素。
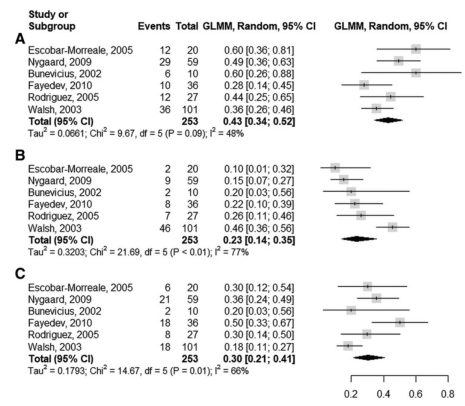
图2 交叉试验中患者偏好的森林图。(A)偏向联合治疗;(B)偏向单一疗法;(C)无偏好。
结论:现有证据表明,LT4/LT3联合治疗和LT4单药治疗治疗成人甲状腺功能减退的临床结果无差异,但有更高比例的患者倾向于联合治疗。两组的不良事件和反应似乎相似,然而,这只是一种观察。这些结果可以为甲状腺功能减退患者和他们的临床医生的用药方案决策提供信息。
原文出处:
Millan-Alanis JM,Gonzalez-Gonzalez JG,Flores-Rodríguez A,et al.Benefits and Harms of Levothyroxine/liothyronine vs. Levothyroxine Monotherapy for Adult Patients with Hypothyroidism: Systematic Review and Meta-analysis.Thyroid 2021 Aug 03
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#利弊#
44
#荟萃#
45
#荟萃分析#
33
路过
41
#单药治疗#
34
#系统综述#
30
#左旋甲状腺素#
42