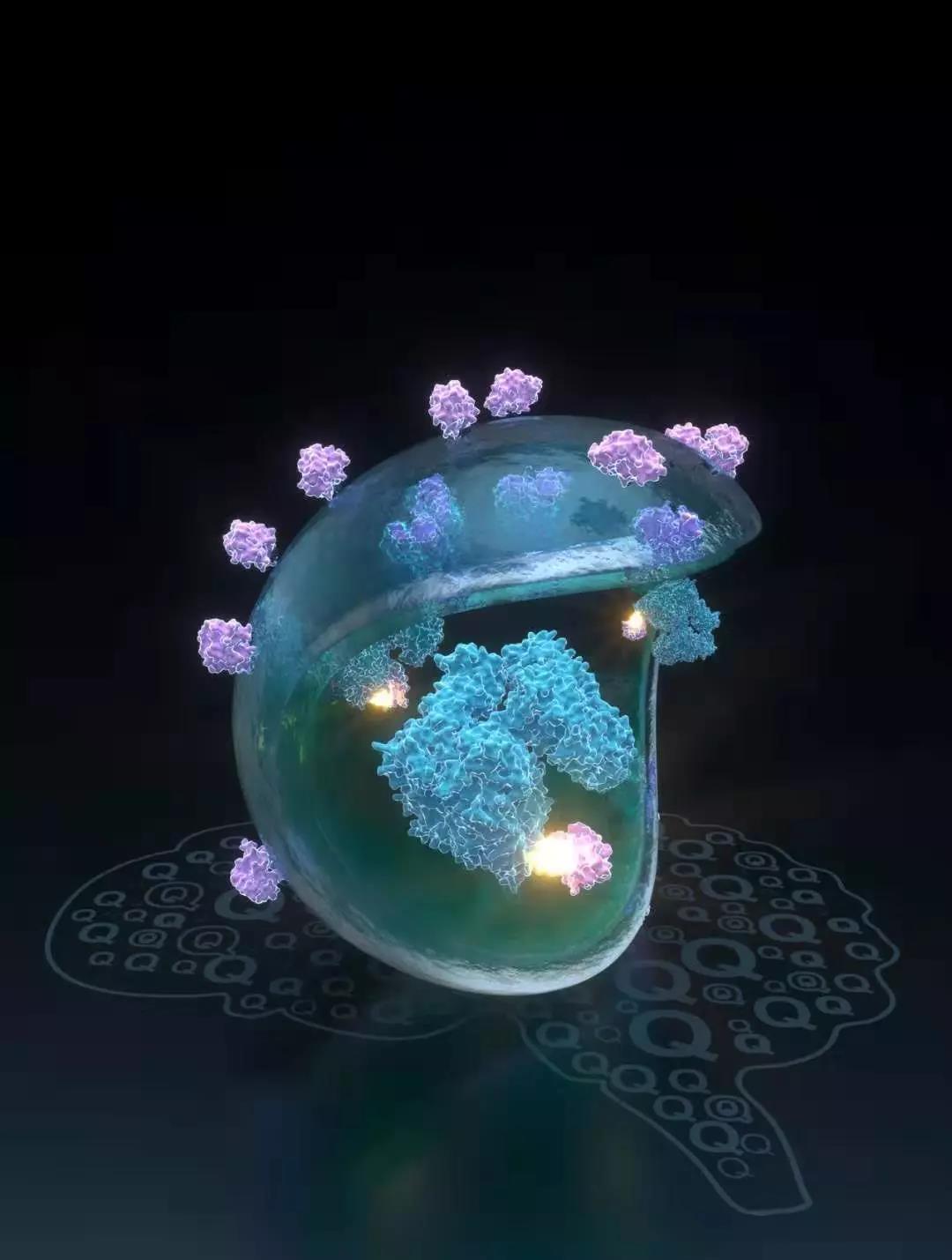
Nature:复旦大学鲁伯埙、丁澦、费义艳团队合作研发亨廷顿病潜在新药
2019-10-31 不详 复旦大学
亨廷顿病(或称亨廷顿舞蹈症)位列四大神经退行性疾病之一,临床表现为不自主的舞蹈样动作、认知障碍、精神异常等症状。由于引起该病的变异亨廷顿蛋白(mHTT)生化活性未知,无法靶向,传统依靠阻断剂以阻断致病蛋白活性的方法并不适用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
32
#研发#
18
#亨廷顿病#
0
#复旦#
31
#亨廷顿#
38