European Radiology:帕金森病的SMwI MRI前瞻性多中心研究
2022-06-06 shaosai MedSci原创
最近,临床上开发了感光图加权成像(SMwI)技术以改善描绘含铁结构的信噪比和对比度-噪声比。最近的研究进一步表明,SMwI在评估3T下的黑质高浓度方面优于SW。
 最近有学者提出,在3T或7T MR的SWI上黑质密度过高或黑质体1可能作为特发性帕金森病(IPD)的一个新的成像标志。一项荟萃分析显示,在3T MR下区分IPD与对照组的集合敏感性和特异性分别为94.6%和94.4%。然而,由于研究入选的患者病程较长、IPD的误诊(5-25%)以及空间分辨率和翻转角度都会影响黑质增生的诊断效果,因此影响到了该技术的广泛应用。
最近有学者提出,在3T或7T MR的SWI上黑质密度过高或黑质体1可能作为特发性帕金森病(IPD)的一个新的成像标志。一项荟萃分析显示,在3T MR下区分IPD与对照组的集合敏感性和特异性分别为94.6%和94.4%。然而,由于研究入选的患者病程较长、IPD的误诊(5-25%)以及空间分辨率和翻转角度都会影响黑质增生的诊断效果,因此影响到了该技术的广泛应用。
最近,临床上开发了感光图加权成像(SMwI)技术以改善描绘含铁结构的信噪比和对比度-噪声比。最近的研究进一步表明,SMwI在评估3T下的黑质高浓度方面优于SW。因此,目前关于SMwI在多中心环境下使用不同供应商的各种MRI扫描仪的结果的数据是有限的。
近日,发表在European Radiology杂志的一项研究在10个不同的中心使用不同的MRI扫描仪上测试了标准化的SMwI与DAT PET在诊断神经退行性帕金森病方面的诊断性能,为该技术的标准化应用流程的建立及推广提供了数据支持。
本研究在2019年11月至2020年10月期间前瞻性地招募了257名受试者,其中包括157名神经退行性帕金森病患者,54名非神经退行性帕金森病患者,以及来自10家医院的46名健康受试者。所有参与者都接受了SMwI和18F-FP-CIT PET检查。SMwI由两名独立审查员解释黑质体1的存在或不存在异常,并通过共识解决差异。 18F-FP-CIT PET被用作参考标准。使用Cohen's kappa系数测试观察者之间的一致性。McNemar's检验用于检验每个参与者和黑质(SN)的SMwI和18F-FP-CIT PET解释之间的一致性。
每个SN和参与者的观察者之间的一致性分别为0.924和0.942。每个SN和参与者的SMwI的诊断敏感性分别为97.9%和99.4%;其特异性分别为95.9%和95.2%,其准确性分别为97.1%和97.7%。SMwI和18F-FP-CIT PET的结果没有显著差异(P>0.05,对SN和参与者而言)。
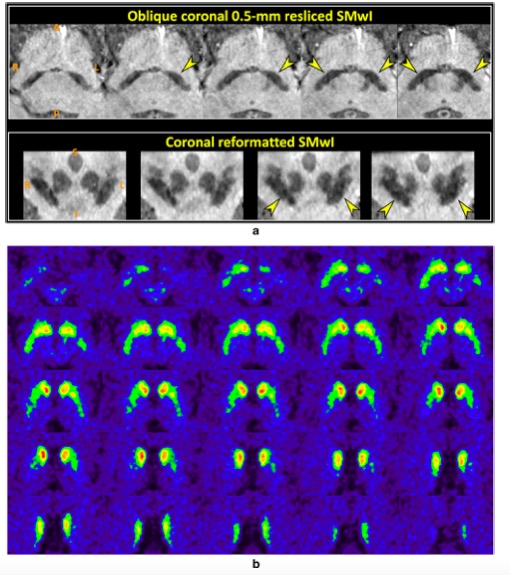
图 71岁的特发性帕金森病女性患者。 a 低信号度区掩盖了黑质两侧的三层(内层低信号、中层高信号和外层低信号度)的分化(上排箭头)。在垂直于中脑的重新格式化的图像上,红核下方的黑质也有相应的异常(下行箭头)。A,前部;P,后部;R,右侧;L,左侧;S,上部;I,下部
本研究表明,在多中心环境下,使用不同的MRI扫描仪确定黑质变性,标准化的高空间分辨率SMwI的诊断性能与18F-FP-CIT PET相当,表明SMwI对于评估帕金森病患者具有普遍性。
原文出处:
Young Hee Sung,Joong-Seok Kim,Sang-Won Yoo,et al.A prospective multi-centre study of susceptibility map-weighted MRI for the diagnosis of neurodegenerative parkinsonism.DOI:10.1007/s00330-021-08454-z
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#多中心研究#
57
#前瞻性#
43
#PE#
37
#多中心#
38