
通常,血压在夜间下降并在醒来时升高,与身体的昼夜节律一致。在一些高血压患者中,不会发生典型的夜间血压下降。这种“夜间血压升高”在 2 型糖尿病患者中很普遍,并且与心血管疾病事件的增加有关。然而,糖尿病夜间血压升高的原因和机制尚不完全清楚。
最近,一项由肯塔基大学医学院发表在PNAS的一项新研究表明,限时饮食可能有助于 2 型糖尿病患者减少夜间高血压(夜间血压升高)。研究发现,限时进食,即每天在特定时间段内进食,有助于预防和改善糖尿病小鼠的夜间高血压。

在该研究中,研究人员将老鼠每天典型的活跃清醒时间限制在八小时内进食。研究员调查了糖尿病db/db小鼠食物摄入时间与血压 (BP) 昼夜节律之间的因果关系。
结果表明,在随意喂食正常食物的糖尿病db/db小鼠中,食物摄入量和血压是紊乱的。通过限时喂养(TRF;食物在活动期仅 8 小时可用),可防止db/db小鼠出现夜间血压升高并有效恢复db/db 中已经被破坏的 BP 昼夜节律。
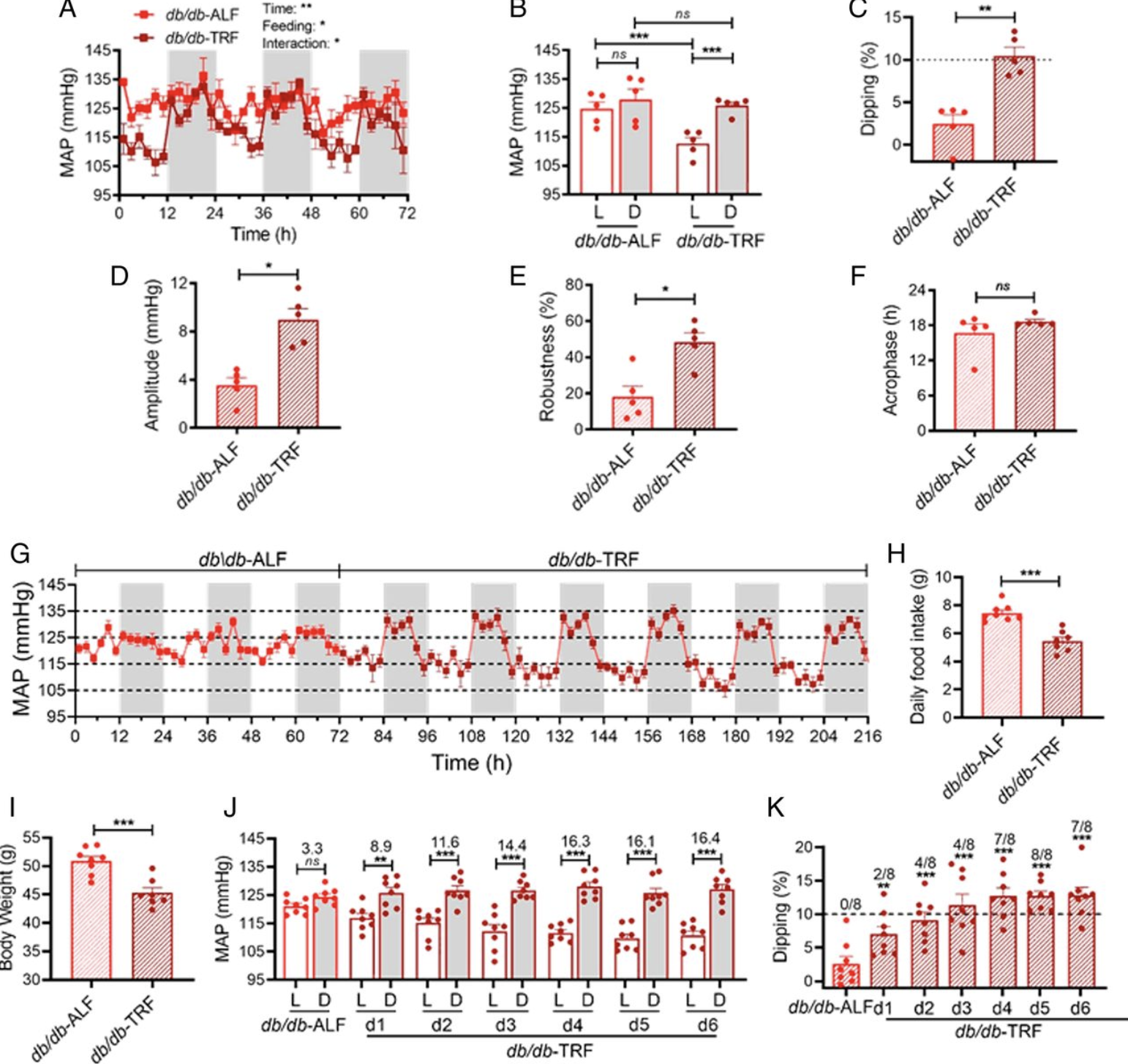 TRF可恢复db/db小鼠的夜间血压下降
TRF可恢复db/db小鼠的夜间血压下降
有趣的是,在db/db小鼠的活跃黑暗阶段将食物供应时间从 8 小时增加到 12 小时,促进了等热量喂养,并且仍然为db/db小鼠的血压昼夜节律提供了强有力的保护。相比之下,8 小时和 12 小时 TRF 都不影响野生型小鼠的血压下降。
这证明影响是由喂食时间而不是卡路里限制引起的。从机制上讲, TRF通过抑制db/db小鼠在不活动和禁食的轻度阶段的交感神经活动来保护 BP 昼夜节律。
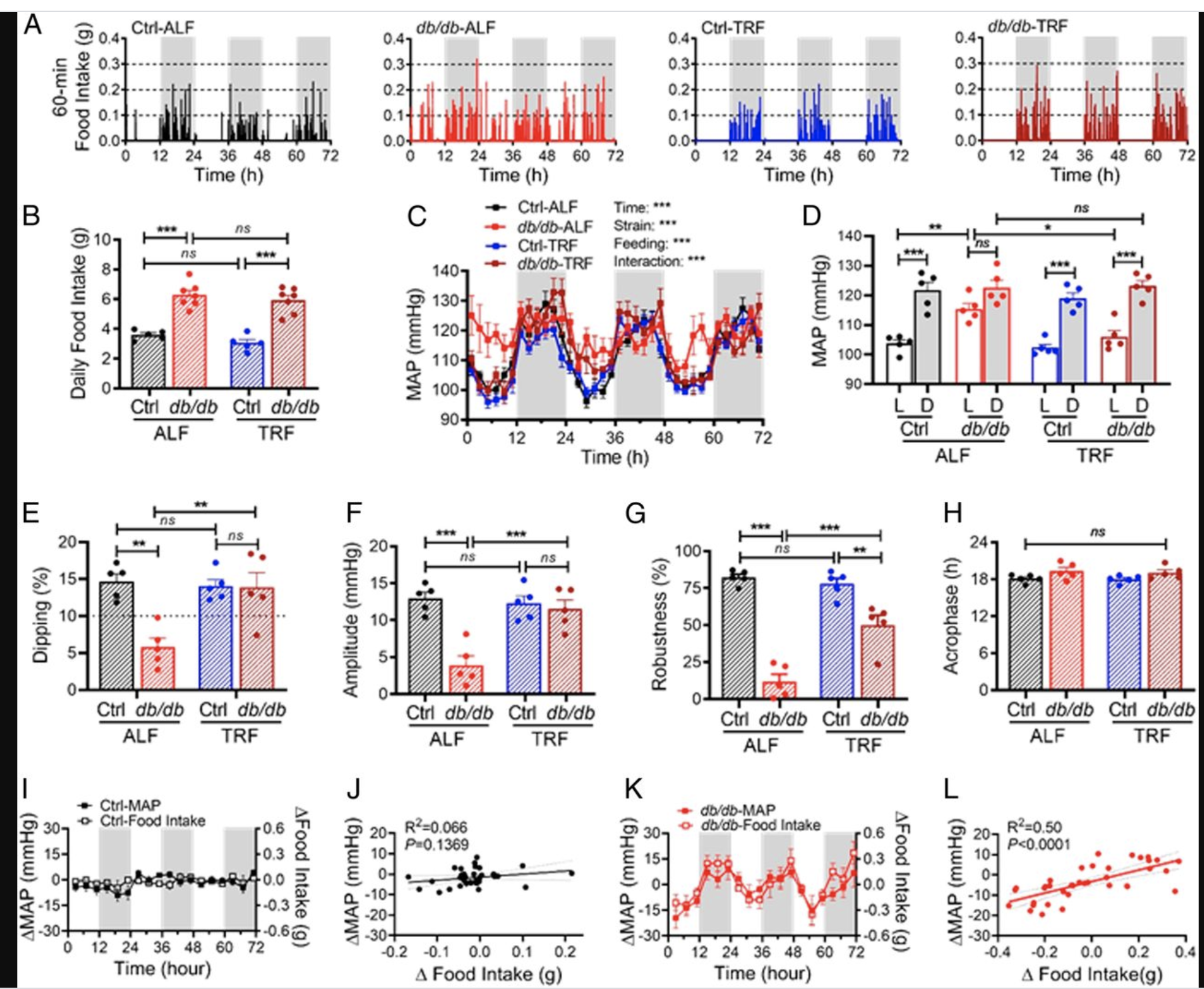 将TRF从8小时增加到12小时仍然可以使db/db小鼠夜间血压下降
将TRF从8小时增加到12小时仍然可以使db/db小鼠夜间血压下降
“我们对这些发现及其对未来临床研究的影响感到兴奋,”郭说。“除了饮食和锻炼等生活方式的改变外,限时饮食可能对 2 型糖尿病患者产生健康影响。”“虽然已经有许多研究表明限时饮食对健康有益,特别是对于代谢问题,”龚说。“但是该研究是第一项基础科学研究,研究限时饮食如何影响与糖尿病相关的夜间血压问题。
总的来说,这些数据揭示了食物摄入时间在预防和治疗糖尿病夜间血压不下降的潜在关键作用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#PNAS#
41
#夜间高血压#
37
#进食#
26
#高血压#学到了
56
学习到了👍
67
谢谢MedSci提供最新的资讯
0
有趣
61