JAHA:妊娠高血压后心律失常增加
2022-01-12 MedSci原创 MedSci原创
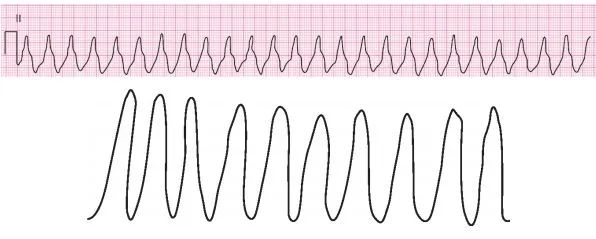
PIH与分娩后1年内心律失常的发生显著相关。然而,PIH并未增加致死性心律失常的发生率。心律失常,尤其是房颤,可能在很大程度上增加了伴有PIH病史女性未来的心血管风险。
妊娠性高血压(PIH)的特征是妊娠20周后出现高血压伴有或不伴有蛋白尿或其他严重特征。它与高血压等心血管疾病(CVD)风险升高和加速发展相关,它们包括血脂异常、心脏衰竭、糖尿病以及冠状动脉、脑血管和外周动脉疾病。尽管妊娠性高血压(PIH)与心血管风险升高有关,但长期研究或孕前基线数据很少。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员使用具有孕前定期健康筛查数据的大型全国性队列探究了PIH后临床上显著的心律失常发病率是否增加。

该研究的数据取自韩国国民健康保险数据库,并结合国民健康检查数据库;对2007年至2015年分娩并在孕前一年内接受过国家健康筛查的女性进行随访至2016年。研究人员排除了孕前1年内诊断为心律失常的女性。该研究的主要结局是分娩后一年内出现明显的心律失常,次要分析仅包括具有临床意义的心律失常的特定诊断代码。此外,研究人员使用硫酸镁对心律失常的风险进行了分层。
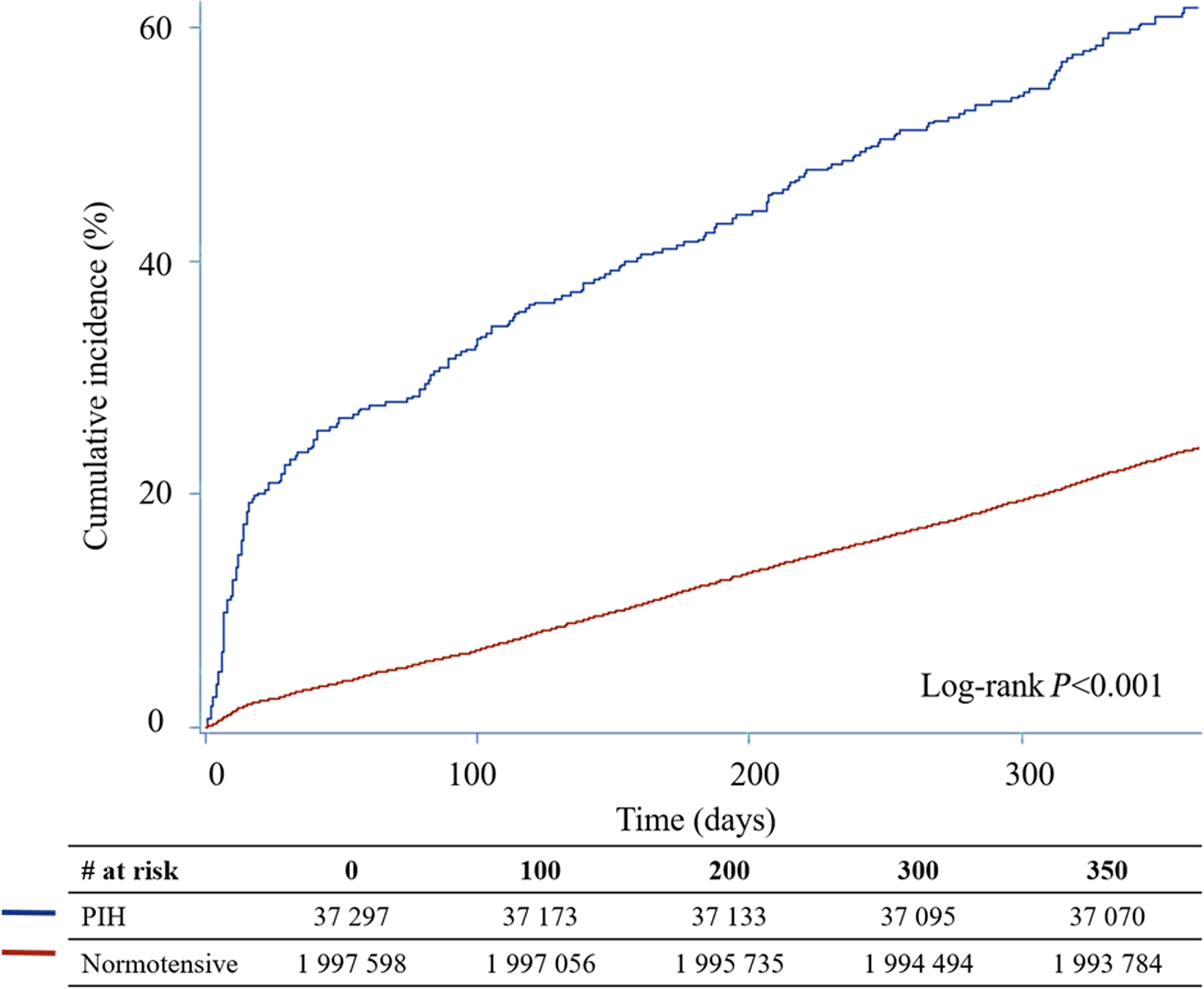
在2035684名女性(PIH;n=37297与血压正常妊娠;n=1998387)中,PIH组的孕前风险较高,且心律失常的发生率高于1年内血压正常妊娠的女性。患有PIH的女性发生房扑/房颤和房室传导阻滞的风险显著增加,但没有致命的心律失常。心律失常发展的其他预测因素包括高龄产妇和剖宫产。分层分析显示使用硫酸镁会增加心律失常的风险。
由此可见,PIH与分娩后1年内心律失常的发生显著相关。然而,PIH并未增加致死性心律失常的发生率。心律失常,尤其是房颤,可能在很大程度上增加了伴有PIH病史女性未来的心血管风险。
原始出处:
Yoonjee Park,et al.Increased Cardiac Arrhythmia After Pregnancy‐Induced Hypertension: A South Korean Nationwide Database Study.JAHA.2021.https://www.ahajournals.org/doi/10.1161/JAHA.121.023013
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











很不错的研究发现,学习了,非常感谢
0
🤰
40
#AHA#
42
很好的研究
56
学习#学习#
57