JCO:Brentuximab Vedotin可显著减少高危型HL儿童患者的放疗剂量且不影响疗效
2021-04-12 MedSci原创 MedSci原创
本妥昔单抗与维多丁结合应用作儿童高危型HL的一线治疗具有较高的耐受性,可显著减少放疗暴露量,并可获得良好的疗效
霍奇金淋巴瘤(HL)儿科患者采用联合治疗的长期无事件生存率接近90%,总生存率(OS)可达到98%-99%。即使是高风险患儿,5年EFS也可达到85%-94%。
本妥昔单抗维多丁(Brentuximab vedotin)是一种有效的抗CD30抗体-药物结合物,已被批准用于成人经典型霍奇金淋巴瘤。但是,目前本妥昔单抗尚未获批用于HL儿童患者。
本研究是一项开放标签、单臂、多中心的一线临床试验,招募了IIB期、IIIB期或IV期的经典型HL患儿(≤18岁),旨在评估本妥昔单抗是否可用于减少经典型霍奇金淋巴瘤儿童和青少年患者的放疗剂量。
根据GPOH-HD2002治疗第3组(TG3),在OEPA/COPDac(长春新碱、依托泊苷、泼尼松和阿霉素/环磷酰胺、长春新碱、泼尼松和达卡巴嗪)方案中,用本伦妥昔单抗维多丁取代长春新碱;两个疗程的AEPA和4个疗程的CAPDAC。所有化疗结束后,仅对早期反应评估(ERA)未获得完全缓解(CR)的淋巴结部位进行残留淋巴结放疗(25.5Gy)。主要目的是评估联合用药的安全性和有效性(ERA时完全缓解),以及3年EFS和OS。
总体上,共招募了77名患者,其中27名(35%)在ERA时获得完全缓解,并且没有接受放射治疗。需放疗的患者接受了个别残留淋巴结组织的放射治疗。
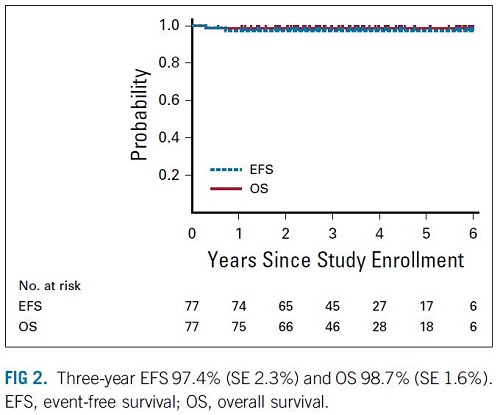
3年EFS和OS
中位随访时间为3.4年,3年EFS为97.4%(SE 2.3%),OS为98.7%(SE 1.6%)。一名接受放疗的患者在治疗结束时发生了疾病的进展,在抢救治疗后6年多仍保持无病状态。发生了一例意料之外的死亡。只有4%的患者发生了3级神经病变。
综上,本妥昔单抗与维多丁结合应用作儿童高危型HL的一线治疗具有较高的耐受性,可显著减少放疗暴露量,并可获得良好的疗效。
原始出处:
Metzger Monika L,Link Michael P,Billett Amy L et al. Excellent Outcome for Pediatric Patients With High-Risk Hodgkin Lymphoma Treated With Brentuximab Vedotin and Risk-Adapted Residual Node Radiation. J Clin Oncol, 2021, undefined: JCO2003286. https://doi.org/10.1200/JCO.20.03286
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JCO#
28
#mAb#
28
又增长了知识
67
显著减少高危儿童患者
51
减少高危儿童
72
#Brentuximab#
36
#vedotin#
33
精彩评论,需要您登录查看
55
谢谢梅斯提供这么好的信息,学到很多
44
学习了,谢谢分享
42