CELL:颜宁组发现儿童遗传神经疾病的结构基础
2020-06-16 MedSci原创 MedSci原创
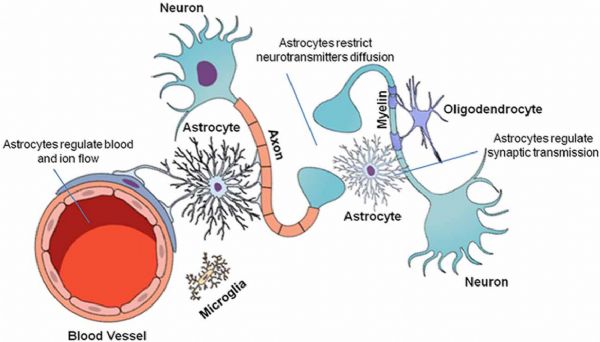
溶酶体胆固醇的排出需要两种蛋白质,NPC1和NPC2,它们的缺陷是导致Niemann-Pick病C型(NPC)的原因。
溶酶体胆固醇的排出需要两种蛋白质,NPC1和NPC2,它们的缺陷是导致Niemann-Pick病C型(NPC)的原因。
最近,颜宁课题组提出了NPC1和NPC2系统的结构表征,揭示了胆固醇从NPC2传递到NPC1的低pH依赖性的跨膜(TM)域的分子基础。
在pH值8.0时,在纳米盘和洗涤剂中分别获得了分辨率为3.6 Å和3.0 Å的NPC1的结构,两者十分类似,揭示了连接N端域(NTD)和跨膜甾醇感应域(SSD)的隧道。
在pH值5.5时,NTD表现出两种构象,表明胆固醇传递到隧道的运动。在隧道的膜边界发现了一个假定的胆固醇分子,TM2向SSD上的表面口袋的形成移动。
最后,在pH5.5的条件下,研究人员获得了4.0 Å分辨率的NPC1-NPC2复合物结构,阐明了胆固醇从NPC2向NPC1(NTD)递送的分子基础。
原始出处:
Hongwu Qian et al. Structural Basis of Low-pH-Dependent Lysosomal Cholesterol Egress by NPC1 and NPC2, CELL (2020). DOI:https://doi.org/10.1016/j.cell.2020.05.020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CEL#
30
#结构基础#
41
#Cell#
32
#颜宁#
53
#神经疾病#
41