BMJ:罕见的胸锁关节脓毒性关节炎——案例报道
2015-11-20 Mechront 译 MedSci原创
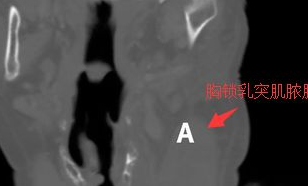
85岁老年女性,克罗恩病的恶化使用免疫抑制剂治疗期间,左肩膀疼痛,且疼痛加剧。肩膀和胸片未见明显异常。随后左颈部出现肿胀红斑。CT:左胸锁关节(SCJ)化脓性关节炎;继发左胸锁乳突肌脓肿(A)和锁骨病理性骨折(B)。如下图。使用免疫抑制的患者,脓毒性关节炎发病率增加。该患者表现为SCJ的脓毒性关节炎,表现为肩膀和胸部疼痛,诊断首选CT。并发症包括了颈部脓肿和纵隔炎。原始出处:Kiruthiga S
85岁老年女性,克罗恩病恶化,在使用免疫抑制剂治疗期间,左肩膀疼痛,且疼痛加剧。肩膀和胸片未见明显异常。
随后左颈部出现肿胀红斑。
CT:左胸锁关节(SCJ)化脓性关节炎;继发左胸锁乳突肌脓肿(A)和锁骨病理性骨折(B)。如下图。
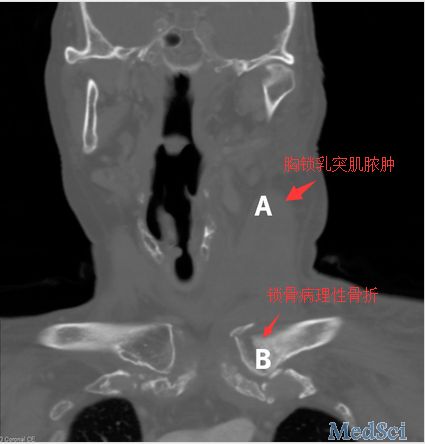
使用免疫抑制的患者,脓毒性关节炎发病率增加。该患者表现为SCJ的脓毒性关节炎,表现为肩膀和胸部疼痛,诊断首选CT。并发症包括了颈部脓肿和纵隔炎。
原始出处:
Kiruthiga Sivakolunthu,Tawakir Kamani.An uncommon case of sternoclavicular septic arthritis.BMJ 2015;351:h4967
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习啦,谢谢分享!
80
#脓毒性#
30
#BMJ#
29
值得关注
130
好文章
138
#关节炎#
23
#罕见#
22