BJU Int:根治性前列腺切除术治疗寡转移性前列腺癌的可行性和安全性评估
2022-01-18 AlexYang MedSci原创
测试了在标准护理(SOC)系统治疗的基础上,随机进行前列腺根治术加盆腔淋巴结切除术(RP)的可行性。
前列腺癌是西方男性最常见的癌症,也是癌症死亡的第二大原因。出现转移性疾病患者的中位生存期为42.1个月,直到最近,护理标准也是最初的雄性激素阻断疗法(ADT)而已。

近期,来自英国的研究人员在《BJU Int》上发表文章,在新诊断为寡转移性前列腺癌的男性中,测试了在标准护理(SOC)系统治疗的基础上,随机进行前列腺根治术加盆腔淋巴结切除术(RP)的可行性。
研究为一项前瞻性、随机、非盲、可行性的临床试验,使用了QuinteT招募干预措施(QRI)来优化招募工作,并在全国九个三级医疗中心进行。在18个月的招募期内,将50名患有寡转移性前列腺癌的男性随机纳入SOC系统治疗与SOC加RP(干预组)。使用了EQ-5D-5L问卷调查获取基线和随机化后三个月的生活质量(QOL)数据;通过常规临床病理评估获取两组的不良事件和前列腺特异性抗原,以及手术组的标准围手术期参数。
结果表明,在176名参与者中,共有71名符合纳入标准,其中51名男性被随机化(其中1人随后确定不合格)。在QRI优化条件下,招募增加率为60-83%。所有参与者均完成了试验随访;干预组的1名参与者随后没有接受手术干预,SOC组的1名参与者拒绝了所有治疗。QOL数据显示,两个研究组的功能性评分都很高。研究发现,对患有寡转移性前列腺癌的男性进行手术是安全的,对早期功能结果的影响与标准适应症手术相似。
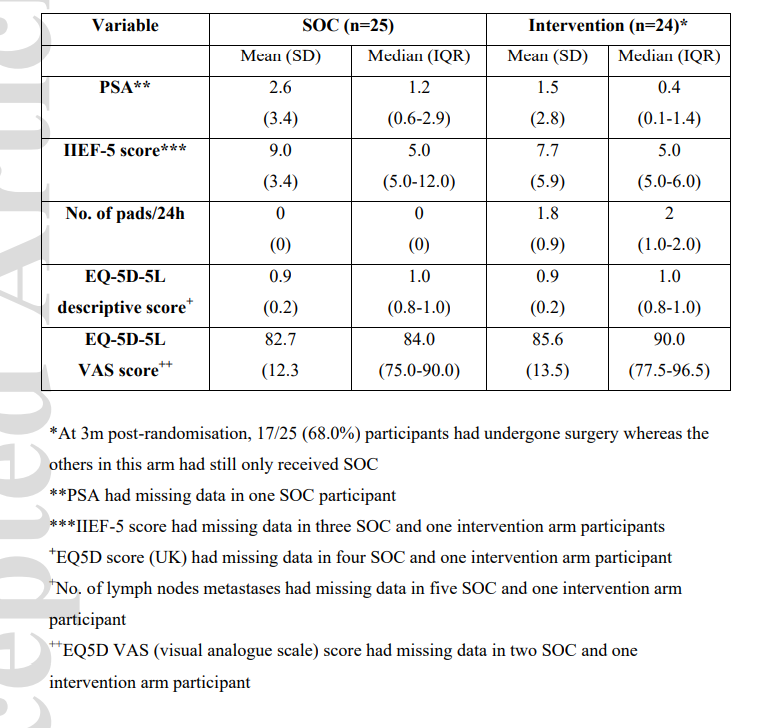
随机化3个月后的PSA、功能和生活质量结果情况
综上所述,在标准的系统治疗之外,对患有同步寡转移性前列腺癌的男性进行随机手术干预是可行的。虽然在这项可行性研究中,手术似乎是安全的,但对QOL没有实质性的影响,但仍必要进行一项大型的随机对照试验,以检测这种多模式管理寡转移性前列腺癌的其他干预措施的治疗效果。
原始出处:
Prasanna Sooriakumaran , Caroline Wilson , Ines Rombach et al. Feasibility and safety of radical prostatectomy for oligo-metastatic prostate cancer: TRoMbone trial. BJU Int. Dec 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#前列腺切除#
41
#切除术#
31
#可行性#
38
#转移性#
32
#转移性前列腺癌#
35
#根治#
28