Blood:吉妥单抗可有效降低NPM1突变型AML患者的复发风险(AMLSG09-09试验)
2020-12-30 MedSci原创 MedSci原创
监测可检测的残留病灶(MRD)可提供核磷蛋白1突变(NPM1mut)型急性髓系白血病(AML)患者的预后信息,是临床试验中评估治疗效果的有力工具。
监测可检测的残留病灶(MRD)可提供核磷蛋白1突变(NPM1mut)型急性髓系白血病(AML)患者的预后信息,是临床试验中评估治疗效果的有力工具。
Silke等人通过定量逆转录PCR反应(RT-PCR)检测NPM1mut转录本水平(TLs),并评估NPM1mut MRD对预后的影响,以及吉妥单抗(GO)对参与AMLSG 09-09随机试验的NPM1mut AML患者的NPM1mut转录本水平和累积复发率(CIR)的影响。
研究人员共分析了469例患者的3733份骨髓(BM)样本和3793份外周血(PB)样本。
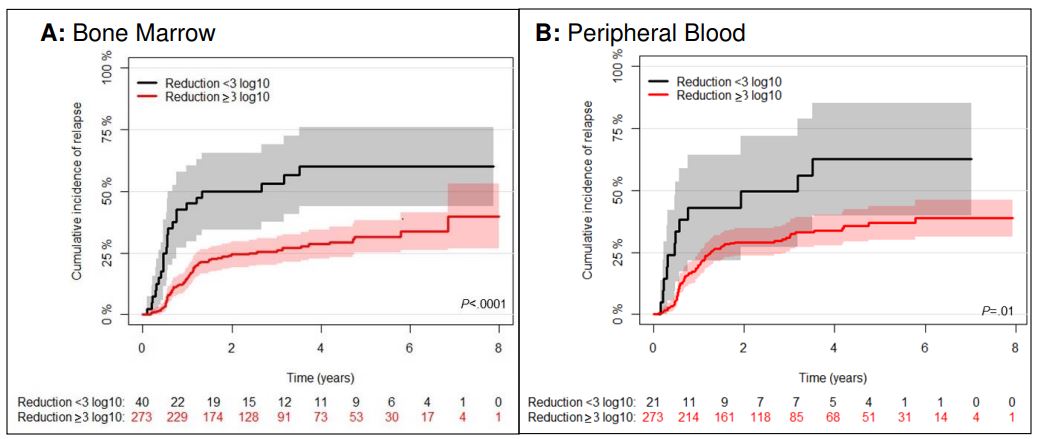
NPM1突变型转录水平降低对2个诱导疗程后的累积复发率的影响
治疗2个周期和治疗结束(EOT)后,骨髓和外周血中NPM1mut的转录水水平降低≥3log10和MRD阴性与低CIR率显著相关(P<0.05)。
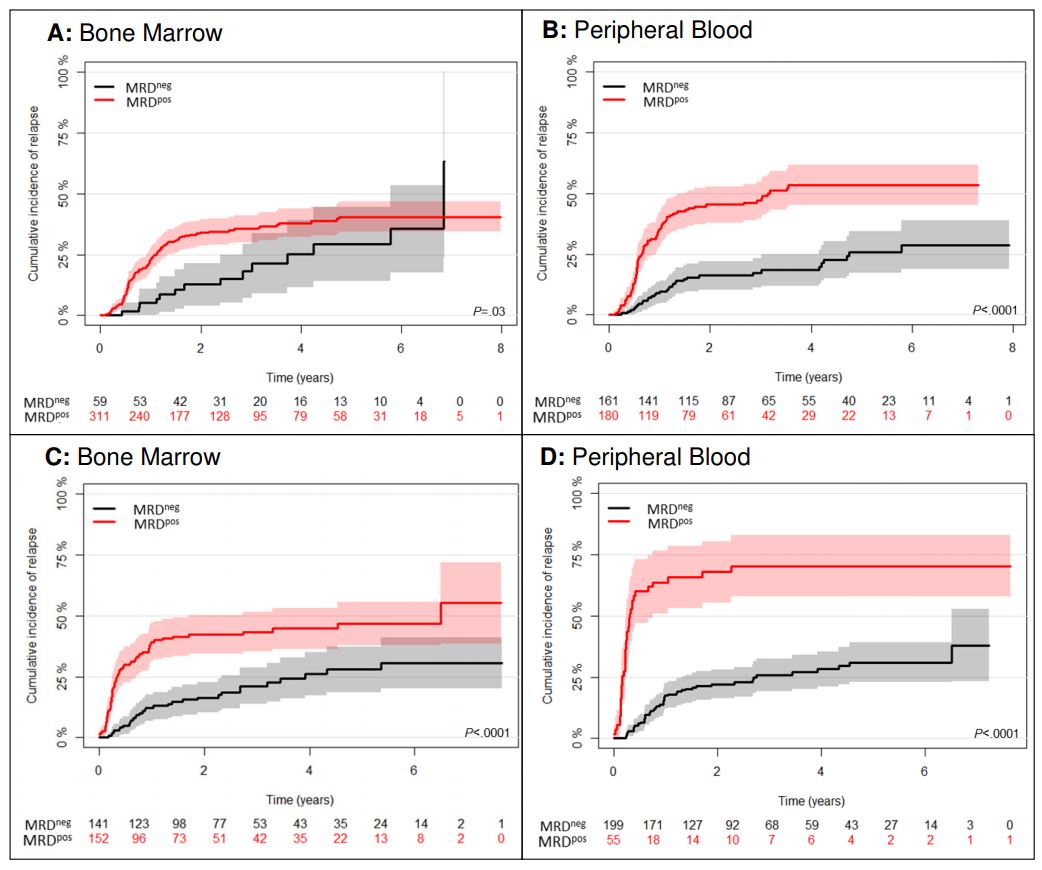
治疗后NPM1突变型MRD阴性对CIR的影响
在多变量分析中,BM和PB样本MRD阳性始终都是预后较差的因素。就治疗效果而言,在所有治疗周期中,GO组中的NPM1mut的中位转录水平显著降低,导致EOT时MRD阴性患者的比例明显增加(56% vs 41%;P=0.01)。
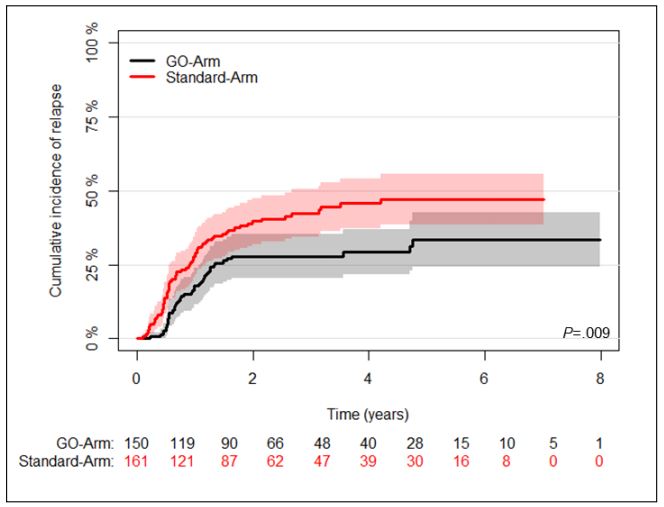
两个治疗组MRD持续阳性患者的CIR
MRD阳性患者加用GO治疗2个周期后,NPM1mut的转录水平明显降低,导致CIR率随之显著降低(4年CIR:29.3% vs 45.7%,P=0.009)。
总而言之,在NPM1mut AML的强化化疗中加入吉妥单抗后,在所有治疗周期中NPM1mut的转录水平均显著减少,患者的复发率也随之显著降低。
原始出处:
Kapp-Schwoerer Silke,Weber Daniela,Corbacioglu Andrea et al. Impact of gemtuzumab ozogamicin on MRD and relapse risk in patients with NPM1-mutated AML: results from the AMLSG 09-09 trial.Blood, 2020, 136: 3041-3050.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PM1#
30
#突变型#
37
#复发风险#
27
#吉妥单抗#
33
#NPM1#
41
看看最新进展
5