JACC:1.4万人双盲随机试验| 不同剂量的依度沙班预防房颤患者卒中的净临床结局
2021-03-06 Nebula MedSci原创
在ENGAGE AF-TIMI 48试验中,低剂量依度沙班(edoxaban)方案(LDER)和高剂量依度沙班方案(HDER)在预防心房颤动卒中的效果不逊于管理良好的华法林。
在ENGAGE AF-TIMI 48试验中,低剂量依度沙班(edoxaban)方案(LDER)和高剂量依度沙班方案(HDER)在预防心房颤动卒中的效果不逊于管理良好的华法林。
本试验目的是在ENGAGE AF-TIMI 48试验中综合比较LDER(30 mg/日,选择性降至15 mg)与HDER(60 mg/日,选择性降至30 mg)的净临床结局(NCO)。
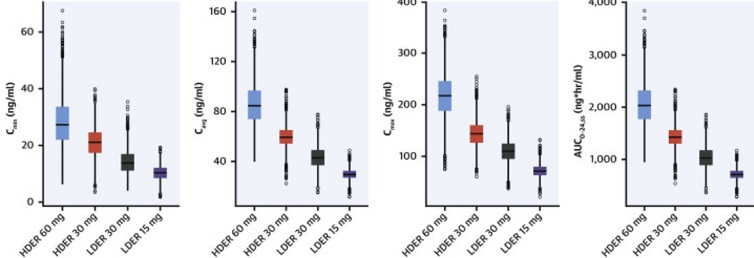
两组依度沙班的血药浓度
两组的主要NCO发生率
LDER组的预定的主要NCO(卒中/全身栓塞[SEE]、大出血、死亡)的发生率较HDER组的低(7.26% vs 8.01%;危险比[HR]:0.9;95%CI 0.84~0.98;P=0.014)。
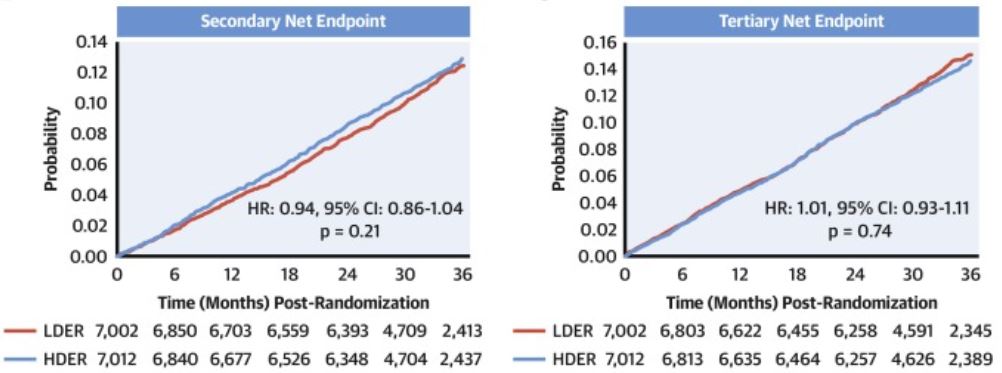
两组的次要和第三NCO发生率
两种给药方案之间的次要(致残性卒中、危及生命的出血或全因死亡)和第三预定的NCO(卒中、SEE、危及生命的出血或全因死亡)相似。
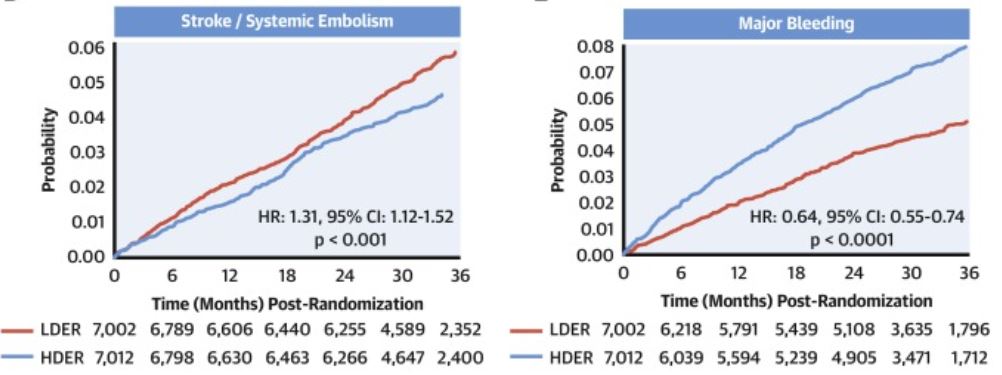
两组的卒中/SEE和大出血发生率
LDER组的患者发生卒中/SEE的风险明显较HDER组的高(2.04% vs 1.56%;HR:1.31;95%CI 1.12%~1.52%;P<0.001)。相反,LDER组的大出血、颅内出血、消化道大出血和危及生命的出血的发生率明显低于HDER组。
总之,在ENGAGE AF-TIMI 48试验中,与HDER相比,LDER组的主要NCO降低,而次要和第三NCO在两种给药方案之间无明显差异。
原始出处:
Steffel Jan,Ruff Christian T,Yin Ophelia et al. Randomized, Double-Blind Comparison of Half-Dose Versus Full-Dose Edoxaban in 14,014 Patients With Atrial Fibrillation. J Am Coll Cardiol, 2021, 77: 1197-1207.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JACC#
45
#依度沙班#
102
#临床结局#
38
#ACC#
36
#随机试验#
40
#双盲#
45
#房颤患者#
43
学习了
89
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
66
房颤,临床上碰到很多哦
67