上颌融合磨牙根管治疗1例报告
2020-03-20 郭佳杰 詹福良 仇丽鸿 中国实用口腔科杂志
融合牙是2颗相邻的牙齿、或正常牙齿与多生牙齿相融合,多见上颌前牙或上颌磨牙与多生牙融合。本文报道的1例上颌第一磨牙与第二磨牙融合伴发根尖周炎病例,在临床中十分罕见。
融合牙是2颗相邻的牙齿、或正常牙齿与多生牙齿相融合,多见上颌前牙或上颌磨牙与多生牙融合。本文报道的1例上颌第一磨牙与第二磨牙融合伴发根尖周炎病例,在临床中十分罕见。
1.病例资料
患者女,19岁,于2016-02-15就诊于中国医科大学附属口腔医院牙体牙髓病科。患者多年前7曾行保髓治疗,治疗后曾有长期根尖酸胀史,1周前患牙出现阵发性胀痛,3d前左侧面颊部肿胀,近2日患牙胀痛逐渐缓解,咬合不适,来诊。
临床检查:67牙冠相连,6牙冠近中倾斜,未见明显牙体病损,叩痛(+),无松动,牙髓电活力测试无反应;7牙冠远中倾斜,面可见充填物,叩痛(+),无松动,牙髓电活力测试无反应,腭侧黏膜可见窦道;67颊侧牙体结合部探及牙周袋深约5mm(图1a~b)。X线根尖片可见67冠根影像交错重叠(图1c);曲面断层片可见67冠部相连,牙根交错(图1d);结合锥形束CT(CBCT)可见67在牙冠颈1/3处融合,6近颊根(MB)可见两根管,远颊根(DB)疑似与7颊根(B)有融合,腭侧可见6腭根(P)及7腭根(P),67根分叉及根尖区可见大面积低密度透射影,腭侧骨壁破坏(图1e~f)。临床诊断:67慢性根尖周炎、融合牙。
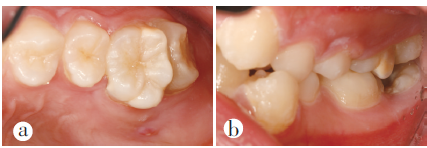


图1a、b治疗前口内像;c治疗前X线根尖片;d治疗前曲面断层片;e、f治疗前CBCT横断面片;
2.临床治疗
一诊:放置橡皮障,去除7面充填物后探及穿髓孔,7开髓后可见髓室内感染严重呈黑色,并伴有臭味溢出,但未见脓液;6开髓后可见冠髓已坏死,10号K锉探查根管,根髓亦无活力;分别插入10号K锉后拍摄X线片,可见6DB指示针疑似与7B指示针存在影像重合(图1g)。67显微镜下探查可见6MB1、MB2、DB、P四根管(图1h),7B、P两根管(图1i)。PathFile疏通根管,ProTapernext结合手用ProTaper根管预备,预备期间结合1%NaClO冲洗及超声荡洗,纸尖拭干根管,Apexcal根管内封药(在行7B根管内封药时可见药物沿6DB根管口溢出,提示7B根管与6DB根管融合连通)(图1j),髓室放置棉球,Caviton暂封;67颊侧连接处牙周刮治,H2O2冲洗,牙周袋内放置盐酸米诺环素软膏。

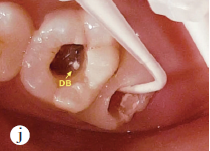
图1g根管探查X线片;h6显微镜下根管口影像;i7显微镜下根管口影像;j7B根管封药可见药物沿6DB根管溢出;
二诊:患者面颊部肿胀消退,67暂封物完好,6叩痛(-)、7叩痛(±),牙龈无红肿,67颊侧连接处牙龈探诊3mm,探诊未见出血,腭侧窦道未愈合。67去除暂封物,1%NaClO冲洗及超声荡洗,纸尖拭干根管,Apexcal根管内封药,Caviton暂封。
三诊:67暂封物完好,6叩痛(-)、7叩痛(-),牙龈无红肿,腭侧窦道未愈合。67去除暂封物,1%NaClO冲洗及超声荡洗,试尖(图1k),VDW热牙胶垂直加压充填(图1l)。67牙冠连接处去净龋坏组织,67面窝洞及牙冠连接处酸蚀,冲洗,粘接,3MZ350树脂充填,调,抛光(图1m)。

图1k根管充填试尖片;l根充后X线片;m根管治疗后口内像;
治疗后3个月复查:患者无自觉症状,67叩痛(-),腭侧窦道口范围减小但未完全闭合,X线片显示根尖区骨密度影像有所增高(图1n~o)。

图1n术后3个月复查X线片;o术后3个月复查口内像;
治疗后12个月复查:患者无自觉症状,67叩痛(-),腭侧窦道基本闭合,X线片显示根尖区骨密度影像显著增高(图1p~q)。
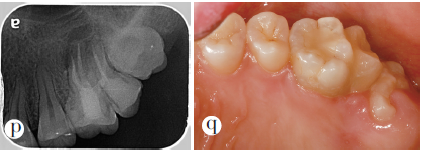
图1p术后12个月复查X线片;q术后12个月复查口内像
3.讨论
融合牙是2颗或多颗发育中的牙齿牙釉质和(或)牙本质间的融合,2颗牙齿的根管系统可以各自独立、也可以出现部分融合,取决于融合时牙齿发育的阶段。本病例根据其临床及影像学表现,最终诊断为67融合牙及慢性根尖周炎。仔细分析患者的病史并结合口内检查可以判断病变始于7的牙髓感染,继而出现牙髓坏死及根尖病变,7感染坏死的牙髓通过B根管与6DB根管系统的融合,导致6继发性牙髓感染。
通过治疗前口内像可以看到患者左侧咬合关系不佳,但6与6尚有咬合接触并且是该侧牙列主要的咀嚼功能牙,若将67一并拔除会严重影响患者的咀嚼功能;也不宜采用分牙拔除术,因为67不仅牙冠融合、在牙根部也存在融合,操作难度大,还易引起牙周问题。因此,综合考虑并结合患者强烈的保牙意愿,遂行67根管治疗。
本病例因67根管系统部分融合,且7牙冠过于向远中倾斜,因此牙髓治疗难度较大。融合牙在行根管治疗前明确其根管解剖特点非常必要。CBCT可以三维立体显示牙髓病变结构,辐射剂量低、空间分辨率高,有助于医生分析牙齿的根管系统或观察目标牙及其周围组织的空间关系。显微镜可以提供充足的光源并放大医生的操作视野,提高牙髓病及根尖周病治疗的成功率。本病例利用CBCT术前分析及显微镜术中放大,判断6DB根管及7B根管存在融合,最终完成根管治疗。
原始出处:
郭佳杰,詹福良,仇丽鸿.上颌融合磨牙根管治疗1例报告[J].中国实用口腔科杂志,2019(03):191-192.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#根管#
29
#融合#
36
#磨牙#
37
#牙根#
41
#上颌#
36