NEJM:原发性高草酸尿症-案例报道
2017-04-13 xing.T MedSci原创
原发性1型高草酸尿症是一种罕见的常染色体隐性乙醛酸代谢紊乱的遗传疾病,导致复发性尿路结石单独或联合肾钙质沉着。支持治疗措施包括高液体摄入,以及口服枸橼酸钾和维生素B6。随访1年,患者尿草酸水平仍然较高,并且多发肾结石。
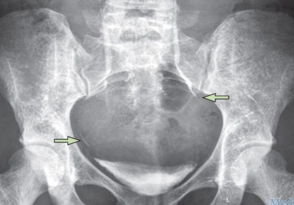
患者为一名3岁的男孩,因6个月的肉眼血尿和间歇性腹痛病史而就诊。尿检可见红细胞,白细胞,和蛋白水平3+。血清肌酐水平为0.9mg/dL(80μmol/L;中国3岁儿童的正常范围为0.3-0.8 mg/dL [20-70μmol/L])。24小时尿草酸盐排泄升高。腹部X线片显示肾脏、膀胱和左侧输尿管内有结石。
排出结石的组分分析表明,结石的组成成分草酸钙一水合物超过95%。结合临床资料,该患者被怀疑为原发性1型高草酸尿症。对AGXT突变分析,AGXT基因编码丙氨酸乙醛酸转氨酶,证实了该患者的诊断。
原发性1型高草酸尿症是一种罕见的常染色体隐性乙醛酸代谢紊乱的遗传疾病,导致复发性尿路结石单独或联合肾钙质沉着。支持治疗措施包括高液体摄入,以及口服枸橼酸钾和维生素B6。
原始出处:
Dapeng Jiang,et al. Primary Hyperoxaluria.N Engl J Med 2017; http://www.nejm.org/doi/full/10.1056/NEJMicm1609986
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#原发性#
49
罕见病例,临床应该参考!
59
学习了,谢谢分享
69
学习了很好的内容
68
少见病例,有利于学习
66