Eur Heart J:心肌纤维化对经导管主动脉瓣植入后左心室重塑、恢复和结局的影响
2020-03-03 xiangting MedSci原创
组织学MF与AS相关性病理LV重塑有关,并独立预测TAVI后的CV死亡率。
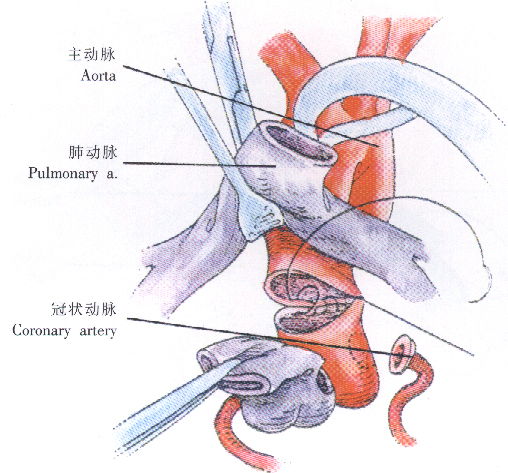
心肌纤维化(MF)在主动脉瓣狭窄(AS)心力衰竭的病理生理中起关键作用。这项研究旨在评估不同的AS亚型患者经导管主动脉瓣植入(TAVI)后,MF对左心室(LV)重塑、恢复和死亡率的影响。
在基线(BL)、TAVI后6个月、1年和2年,对100名严重AS患者进行了前瞻性临床和超声心动图检查。放置瓣膜后收集左心室活检。在Masson三色染色后评估心肌纤维化,并以占总组织面积的百分比计算纤维化面积。根据MF高于(MF+)或低于(MF-)百分比中位数(≥11%或<11%)对患者进行分层。
不同AS亚型间的心肌纤维化负担有显著差异,低射血分数(EF)、低梯度AS的纤维化负担水平最高,而正常EF、高梯度AS的水平最低(29.5±26.4%vs. 13.5±16.1%,P=0.003)。在整个队列中,MF+与LV功能更差、病理性LV重塑程度高以及BL时临床心衰更明显显著相关。TAVI后,MF+与LV几何形状和功能的正常化延迟相关,但本身与不存在逆重塑和临床改善不相关。但是,有22例患者在随访期间死亡(平均11个月),其中14例死亡被归类为心血管(CV)(心律不齐相关性n=9)。重要的是,14例CV死亡中有13例发生在MF+患者(MF+患者的CV死亡率为26.5%,而MF-患者为2%,P=0.0003)。多因素分析确定MF+是CV死亡率的独立预测因子[危险比(HR)27.4(2.0–369),P=0.01]。
组织学MF与AS相关性病理LV重塑有关,并独立预测TAVI后的CV死亡率。
原始出处:
Miriam
Puls. Impact of myocardial fibrosis on left ventricular remodelling, recovery,
and outcome after transcatheter aortic valve implantation in different
haemodynamic subtypes of severe aortic stenosis. Eur Heart J. 12 February 2020.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#经导管主动脉瓣植入#
25
#肌纤维#
26
#主动脉瓣#
30
#ART#
22
#左心室#
28
#主动脉#
0
#经导管#
25
#植入#
29
#HEART#
23