Circulation:原发性心肌纤维化可能是遗传性心脏结构性疾病的替代表型
2018-06-20 MedSci MedSci原创
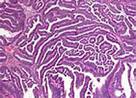
心肌纤维化是年轻人突发心源性猝死后尸检的常见发现。鉴于现尚无明确原因,研究人员推测心肌纤维化在某种程度上是由于缺乏可鉴别的与遗传突变相关的病因(原发性心肌纤维化[PMF])。研究人员从芬兰北部突发性心源性猝死的4031位个体获得尸检组织,在其中145位中仅有PMF这一结构发现。尸检时未找到心肌纤维化的继发原因时,研究人员用靶向二代测序对174个与心肌结构和离子通道功能相关的基因进行测序。根据美国医
研究人员从芬兰北部突发性心源性猝死的4031位个体获得尸检组织,在其中145位中仅有PMF这一结构发现。尸检时未找到心肌纤维化的继发原因时,研究人员用靶向二代测序对174个与心肌结构和离子通道功能相关的基因进行测序。根据美国医学遗传学共识指南,所有对蛋白有影响的等位基因频率<0.01的突变被标记为致病突变或意义不明确的突变。
在96份通过DNA质量控制(66%)的样本中,死后遗传学检测在26个(27%)个体中发现24个已知或意义不明确的突变。10个(10%)个体携带的10个突变为致病或可能致病突变,16个(17%)个体携带的14个突变为意义不明确的突变(位于11个基因上)。5个突变是在与致心律失常性右心室心肌病相关的基因上,11个是在与扩张型心肌病相关的基因上;2个与上述异常均不相关。4个意义不明确的特殊突变在多个独立的PMF个体中表现为共分离。在离子通道编码基因上未发现致病/可能致病的突变。
有很大一部分的PMF个体在尸检时可在致心律失常性右心室心肌病、扩张型心肌病和肥厚行相关的基因上发现突变,但尸检时未发现上述疾病,提示PMF可能是结构性疾病相关基因突变表达的变化表型,或与风险相关的纤维化发生于上述原发性疾病前。本研究发现对尸检基因检测和家系风险分析具有临床指导意义。
原始出处:
M. Juhani Junttila,et al. Primary Myocardial Fibrosis as an Alternative Phenotype Pathway of Inherited Cardiac Structural Disorders. Circulation.June 19,2018.https://doi.org/10.1161/CIRCULATIONAHA.117.032175
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#结构性#
0
#遗传性#
22
#原发性#
25
#肌纤维#
30
#表型#
33
#心脏结构#
41