JAMA:接受机械通气的严重中风患者,早期与标准方法的气管切开对功能恢复的影响
2022-05-12 网络 网络
在接受机械通气的严重中风患者中,早期气管切开的策略与标准的气管切开方法相比,并没有明显改善6个月后无严重残疾的存活率。
许多严重中风患者的气道保护性反射功能受损,导致有创机械通气时间过长。尽管一般危重病人中有15%最终需要气管切开,但在对急性脑损伤(如严重中风)病人的研究中,气管切开率高达35%。
为了检验早期气管插管与标准气管插管是否能改善接受机械通气的中风患者的功能结局,来自德国海德堡大学的学者开展了一项随机临床试验,纳入382名接受有创通气的严重急性缺血性或出血性卒中患者被随机分配(1:1)到早期气管切开术(插管≤5天)或正在进行的呼吸机断流术,结果发表在近期JAMA上。
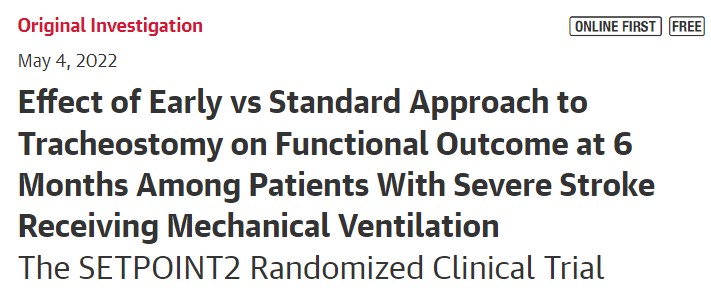
患者在26个美国和德国的神经重症监护中心被随机分配。患者被分配到早期气管插管策略(n = 188)或标准气管插管(对照组)策略(n = 194)。主要结果是6个月时的功能结果,根据改良的Rankin量表评分(0-6),将0(无残疾)至4(中度残疾)与5(严重残疾)或6(死亡)进行二分法计算。
结果显示,在382名随机患者中(中位年龄59岁;49.8%为女性),366名(95.8%)完成了试验,并有主要结果的随访数据(早期组177名患者[94.1%];标准组189名患者[97.4%])。早期气管切开组中95.2%的患者在插管后4天内(IQR,3-4天)进行了气管切开(主要是经皮),对照组中67%的患者在插管后11天内(IQR,10-12天)。
早期气管插管组与对照组相比,6个月时没有严重残疾(mRS评分,0-4)的比例没有显著差异(43.5% vs 47.1%;差异,-3.6% [95% CI,-14.3%至7.2%];OR=0.93 [95% CI,0.60-1.42];P = 0.73)。在严重不良事件中,早期气管切开组有5.0%(121个报告事件中的6个),而3.4%(118个报告事件中的4个)与气管切开有关。
在接受机械通气的严重中风患者中,早期气管切开的策略与标准的气管切开方法相比,并没有明显改善6个月后无严重残疾的存活率。然而,效果估计值周围的置信区间较宽,可能包括了临床上的重要差异,因此不能排除早期气管切开策略带来的临床相关益处或危害。
参考文献:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#气管切开#
40
#学习##心血管#
79
不错的进展,学习
65
#中风患者#
46
#功能恢复#
61
JAMA上文章都是顶级的,谢谢梅斯及时上新
26