三大队列超25年随访研究:都说全谷物可防冠心病,哪一种最给力?有一种还竟会「帮倒忙」?
2022-06-16 MedSci原创 MedSci原创
BMC Med:全谷物食品的摄入和美国男性和女性患冠心病的风险
冠心病(CHD)仍然是美国死亡的主要原因之一。CHD在很大程度上可以通过采用健康的生活方式和饮食来预防。在许多可改变的饮食因素中,全谷物已经被广泛研究与冠心病风险的关系。大多数流行病学研究通过总结所有食物来源的全谷物含量得出全谷物总摄入量,大多数前瞻性队列研究一致记录了整体全谷物消费对预防CHD的实质性健康益处。
然而,很少有研究专门研究个别全谷物食品与CHD风险之间的关系。鉴于谷物物种的各种生化成分,以及在食品制备过程中引入的外源性成分,不同的全谷物食品可能对心血管健康产生不同的影响。最近对流行病学研究的荟萃分析一致表明,全麦食品以及几种全麦食品(包括全麦冷早餐麦片、全麦面包和添加麸皮)的心脏保护作用,而与其他常食用的全麦食品(如糙米、燕麦片和爆米花)的关联和剂量反应关系在很大程度上仍不为人知。

为了填补知识空白,本研究系统地评估了几种常见消费的全谷物食品的摄入量之间的关联,包括全麦冷早餐谷物,燕麦片,黑面包,糙米,爆米花,小麦胚芽和添加麸皮,以及三个大型前瞻性队列的CHD风险,这些队列在三十年的随访中反复评估了饮食和疾病状况。

自1986年以来,本研究跟踪了74244名来自护士健康研究的女性,自1991年以来来自护士健康研究II的91430名女性,以及自1984年以来来自卫生专业人员随访研究的39455名男性,参与者在基线时没有心血管疾病或癌症病史。自基线以来,每2-4年使用经过验证的半定量食物频率问卷反复评估七种个体全谷物食品的摄入量。通过审查医疗记录或死亡证明来确定冠心病的诊断。
结果显示,在平均25.8年的随访期间,记录了9461例冠心病病例。在多变量调整模型中,与每份/天总全谷物消费量相对应的CHD风险的合并风险比(HR)(95%CI)为0.93(0.90-0.95;p 趋势<0.0001)。大多数个体全谷物食品的较高消费量与CHD风险显着降低有关。将每天食用≥1份的参与者与每月食用<1份的参与者进行比较,CHD的多变量调整合并HR(95%CI)为全麦冷早餐谷物0.83(0.78-0.89),黑面包为0.92(0.86-0.99),爆米花为1.08(0.96-1.22)。
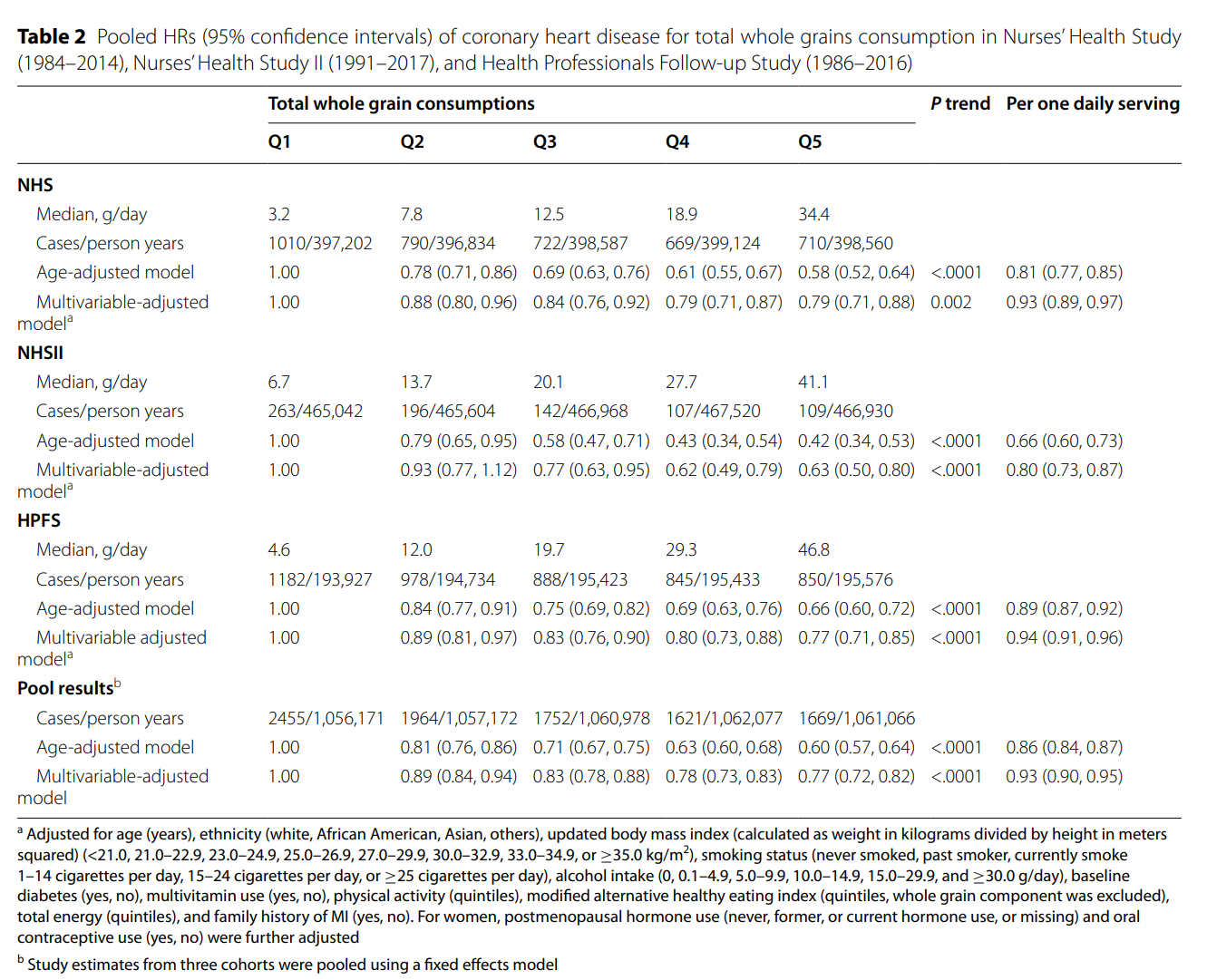
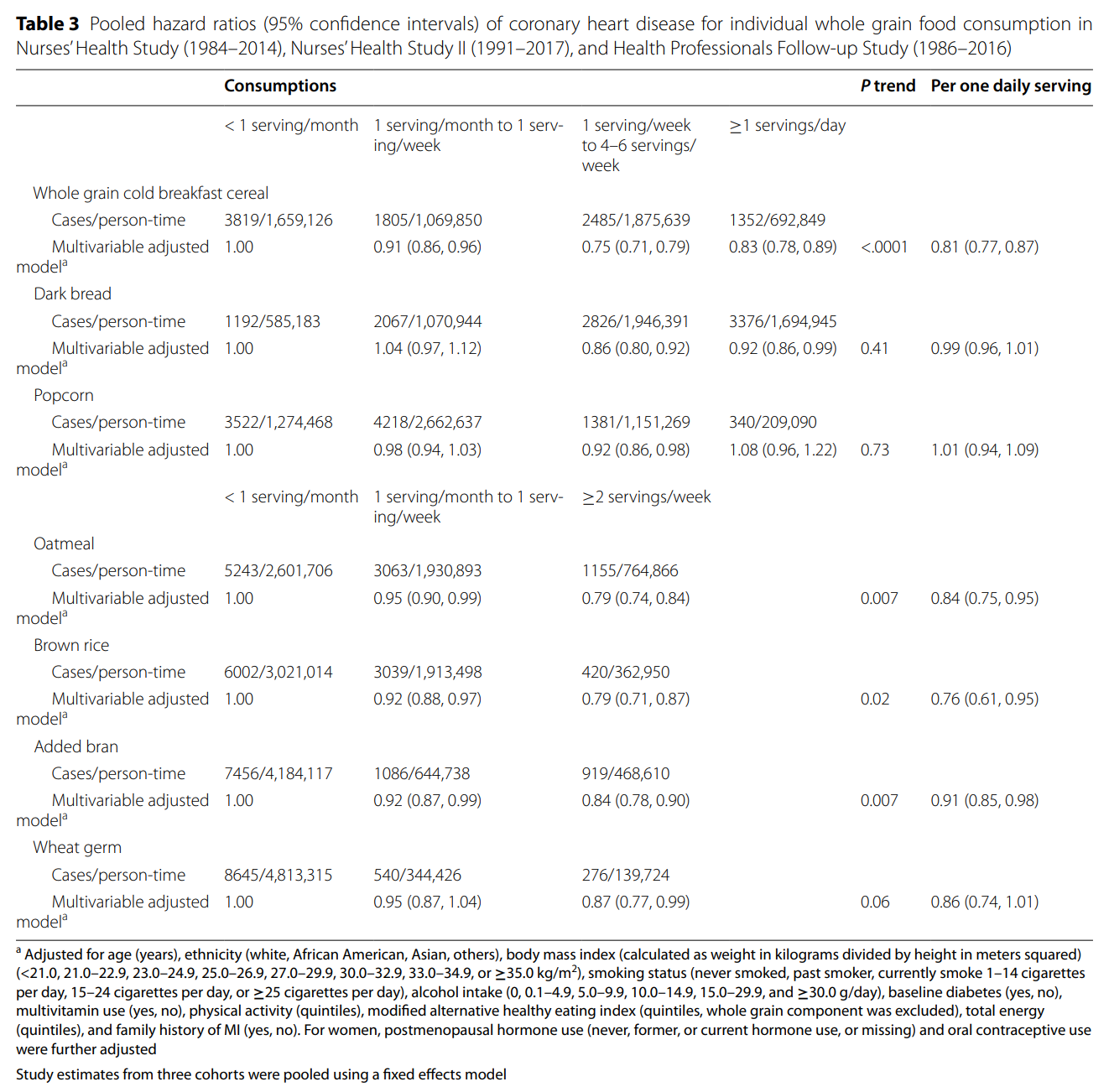
对于其他总摄入量较低的全谷物食品,将每周≥2份的摄入量与每月<1份进行比较,合并的风险比(95%CI)为燕麦片0.79(0.74-0.84),糙米为0.79(0.71-0.87),添加麸皮为0.84(0.78-0.90),小麦胚芽为0.87(0.77-0.99)。立方样条回归表明某些全谷物食品的风险降低约为2份/天,冷早餐谷物和黑面包的风险降低约为0.5份/天,燕麦片为0.5份/周,糙米为1份/周,添加麸皮的风险降低为2份/周(非线性<所有关联的p为0.01)。
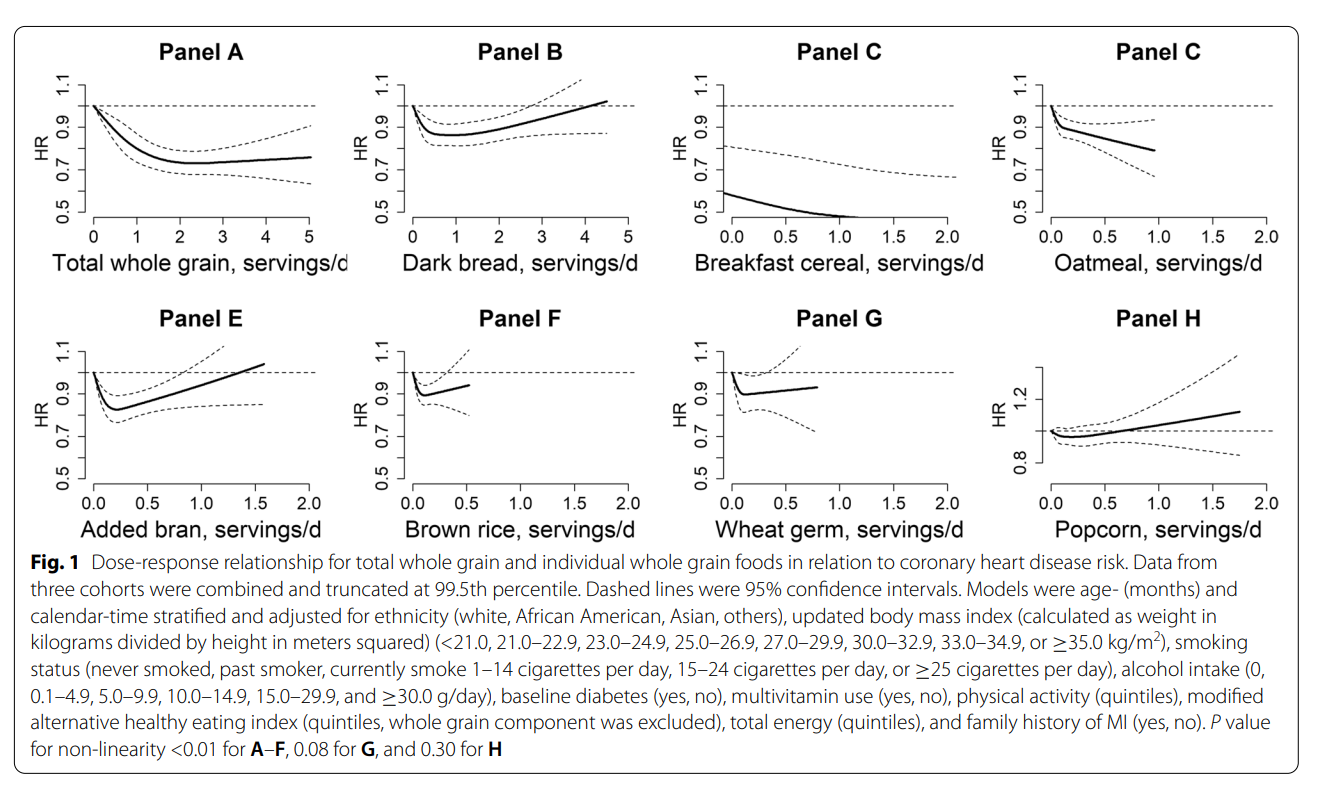
总的来说,这些数据表明,总全谷物的消费量增加,以及除爆米花外的个别全谷物食品,与较低的CHD风险显着相关。在总全谷物和个体全谷物食品的不同摄入量水平下,反关联可能趋于平稳。这项研究提供了进一步的证据,支持增加全谷物摄入量以预防美国人群的CHD。
原文来源:
Hu Y, Willett WC, Manson JAE, Rosner B, Hu FB, Sun Q. Intake of whole grain foods and risk of coronary heart disease in US men and women. BMC Med. 2022;20(1):192. Published 2022 Jun 10. doi:10.1186/s12916-022-02396-z.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#谷物#
39
#5年随访#
51
#随访研究#
50
去关注下原文
47