Movement Disorder:新药Mevidalen治疗路易体痴呆,疗效如何
2022-01-17 MedSci原创 MedSci原创
Mevidalen利用一种新的作用机制,在标准护理的基础上改善与LBD相关的运动症状
路易体痴呆(Lewy body dementia),包括帕金森病痴呆(PDD)和路易体痴呆(DLB),是继阿尔茨海默病(AD)之后第二种最常见的神经变性痴呆。整个皮层下和皮层脑区的路易体内含物,主要包含错误折叠和聚集的α-突触核蛋白,是LBD的组织病理学标志。
 虽然曾经被认为是两个独立的实体,但支持性的病理、临床、影像和神经化学数据的组合表明PDD和DLB属于同一大类疾病。它们有共同的神经影像学特征,有重叠的萎缩模式、葡萄糖利用和神经递质变化(皮质胆碱能障碍和纹状体/皮质多巴胺能障碍)。路易体的形成和传播伴随着进行性的神经变性,特别是影响多巴胺能和胆碱能神经元,导致PDD和DLB的运动和认知障碍的重叠。PDD和DLB都存在进行性的执行功能障碍和视觉空间异常,但在疾病过程的早期,外显记忆仍然相对完整。此外,PDD和LBD的非运动特征相似,包括快速眼动(REM)睡眠行为障碍、嗅觉减退、突出的视觉幻觉、唤醒波动和嗜睡、自主神经功能紊乱和抑郁/焦虑。
虽然曾经被认为是两个独立的实体,但支持性的病理、临床、影像和神经化学数据的组合表明PDD和DLB属于同一大类疾病。它们有共同的神经影像学特征,有重叠的萎缩模式、葡萄糖利用和神经递质变化(皮质胆碱能障碍和纹状体/皮质多巴胺能障碍)。路易体的形成和传播伴随着进行性的神经变性,特别是影响多巴胺能和胆碱能神经元,导致PDD和DLB的运动和认知障碍的重叠。PDD和DLB都存在进行性的执行功能障碍和视觉空间异常,但在疾病过程的早期,外显记忆仍然相对完整。此外,PDD和LBD的非运动特征相似,包括快速眼动(REM)睡眠行为障碍、嗅觉减退、突出的视觉幻觉、唤醒波动和嗜睡、自主神经功能紊乱和抑郁/焦虑。
LBD是一种多方面的疾病,具有核心的运动和非运动特征,常常导致在平衡症状疗效和药物副作用的情况下使用多种药物。标准多巴胺能疗法的使用受到非运动并发症的限制,往往导致运动症状治疗不足,而利伐斯汀(rivastigmine)仍然是美国唯一批准用于治疗PDD认知障碍的药物。
Mevidalen(LY3154207)代表了一种新的机制,是多巴胺D1受体亚型(D1PAM)的选择性正性异生调节剂(PAM)。它的作用是增加D1受体的张力及其对多巴胺的亲和力,从而在多巴胺释放的时间和地点放大对多巴胺的反应。D1受体激动剂在其存在的整个过程中激活它们所能接触到的所有D1受体,并且由于高剂量时的过度刺激和耐受性发展的趋势,常常显示出钟形的剂量反应关系。
相反,Mevidalen通过增强对剩余脑多巴胺(或管理的左旋多巴)的反应,将受到正常反馈控制,过度刺激的倾向较低。梅维达伦有可能通过增强额叶多巴胺能神经递质、激活皮质神经元、增强突触可塑性和D1介导的增强乙酰胆碱释放来改善认知表现。在mevidalen的临床前和一期试验中观察到的其他潜在效果,如减少日间困倦、增强运动功能、改善情绪和目标导向行为,从而减少冷漠(通过激活皮质和纹状体的D1受体),也将有利于LBD。
藉此, Indianapolis - Eli Lilly and Company的Kevin Biglan等人,利用(PRESENCE;NCT03305809)临床试验,评估mevidalen对轻度至中度IBD(PDD或DLB)患者的安全性和疗效与安慰剂相比。主要目标是测试假设,每天服用10、30或75毫克的mevidalen治疗12周,将导致认知能力的明显改善。次要目标旨在评估mevidalen治疗对LBD的运动和非运动方面的影响。
PRESENCE是一项为期12周的2期研究,将LBD患者(N = 344)随机分配(1:1:1:1)到每日剂量的mevidalen(10、30或75毫克)或安慰剂中。
主要结果衡量标准是认知药物研究的注意力连续性(CoA)综合得分从基线的变化。次要结果包括阿尔茨海默病评估量表-认知分量表13(ADAS-cog13)、运动障碍协会-统一帕金森病评分表(MDS-UPDRS)和阿尔茨海默病合作研究-临床全局变化印象(ADCS-CGIC)。
他们发现:Mevidalen未能达到主要或次要认知终点。Mevidalen使MDS-UPDRS总分得到明显的、剂量依赖性的改善(与安慰剂相比,I-III部分之和,10毫克P<0.05,30毫克P<0.05,75毫克P<0.01)。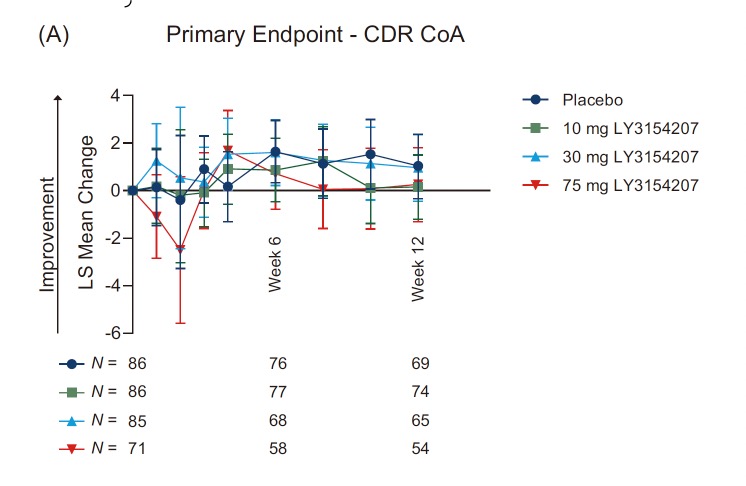
与安慰剂相比,30毫克和75毫克的mevidalen剂量明显改善了ADCS-CGIC的得分(最小或更好的改善:30毫克P<0.01,75毫克P<0.01;中度或更好的改善:30毫克P<0.05,75毫克P<0.001)。
血压、不良事件和心血管严重不良事件的增加在75毫克的剂量下最为明显。
该研究的重要意义在于发现了:Mevidalen利用一种新的作用机制,在标准护理的基础上改善与LBD相关的运动症状,同时改善或不加剧与传统多巴胺能疗法相关的非运动症状。
原文出处:
Biglan K, Munsie L, Svensson KA, et al. Safety and Efficacy of Mevidalen in Lewy Body Dementia: A Phase 2, Randomized, Placebo‐Controlled Trial. Mov Disord. Published online December 2, 2021:mds.28879. doi:10.1002/mds.28879
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#disorder#
43
#Disord#
35
#路易体#
42
#Dis#
32
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
41