Dig Dis Sci:甲磺酸萘法莫他对预防内镜后逆行胰胆管造影术胰腺炎无效
2021-01-27 MedSci原创 MedSci原创
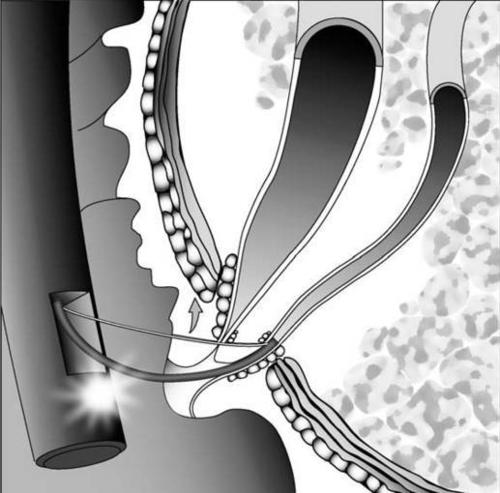
内镜逆行胰胆管造影术(ERCP)是一项重要的内镜技术,目前在全世界范围内用于治疗胰胆管疾病。ERCP的并发症主要包括胰腺炎,出血,胆管炎,胆囊炎和穿孔。
内镜逆行胰胆管造影术(ERCP)是一项重要的内镜技术,目前在全世界范围内用于治疗胰胆管疾病。ERCP的并发症主要包括胰腺炎,出血,胆管炎,胆囊炎和穿孔。在这些并发症中,ERCP术后胰腺炎(PEP)是最常见的,发生率约为2-15%。而蛋白酶抑制剂具有通过抑制胰腺泡细胞中胰蛋白酶原向胰蛋白酶的转化的作用并预防随后的炎症来预防PEP的发生。其中蛋白酶抑制剂——萘莫司他甲磺酸盐(6-脒基-2-萘基对-胍基苯甲酸酯二甲烷磺酸酯; NM)的疗效目前存在较多的争议。因此,需要一个针对NM在PEP中的预防功效的多中心随机对照试验进行证实。
研究人员在这项多中心前瞻性研究中,纳入2012年12月至2019年3月之间计划进行ERCP的800例,年龄≥20岁的患者。主要观察结果是未接受NM(非NM)的患者的PEP的发生率和严重程度与接受NM治疗的患者之间的差异(NM: 20毫克/天)。次要观察结果包括PEP的危险因素以及与NM相关的不良事件。
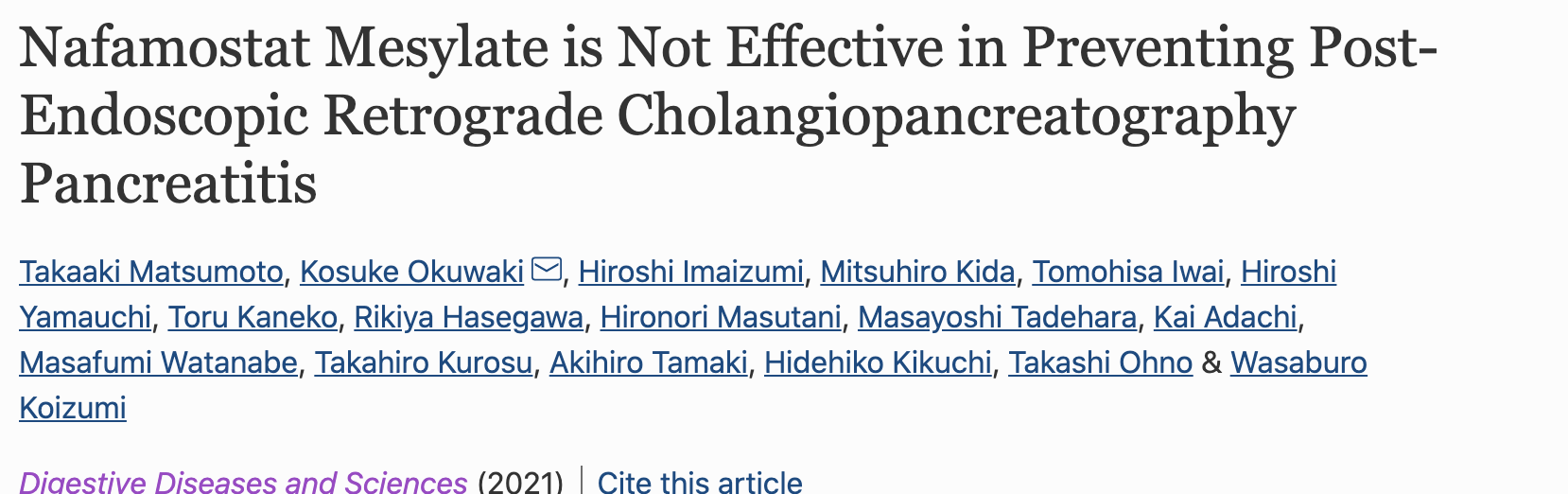
800名患者中仅有441被纳入本项研究(非NM:n= 149; NM:n = 292)。患者特征在基线时保持相对平衡,各组之间无显着差异。总PEP发生率为40/441(9%),(非NM:n = 15 [10%]; NM:n = 25 [9%])。在接受NM治疗组中,PEP的发生率在低风险组比高风险组低。胰腺穿刺和双导线引流技术是PEP的独立危险因素。NM相关的高钾血症等不良事件的发生率为0.7%。
本项研究证实NM对PEP有预防作用,而与给药时间无关,但是,还需要进一步研究。
原始出处:
Takaaki Matsumoto. Et al. Nafamostat Mesylate is Not Effective in Preventing Post-Endoscopic Retrograde Cholangiopancreatography Pancreatitis. Digestive Diseases and Sciences.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#造影术#
49
#Dis#
50
是我理解错了 结论和题目有点冲突?
98
#内镜#
49
#造影#
33
#胆管#
35