Front Oncol:复发鼻咽癌患者挽救手术治疗的疗效:meta分析
2021-10-17 yd2015 MedSci原创
该荟萃分析表明,复发鼻咽癌患者挽救性手术有利于生存。准确评估肿瘤的复发分期和选择合适手术方式是成功关键。后期需要更多的随机对照研究去进一步证实。
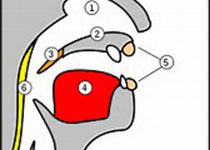
鼻咽癌是一种发生于头颈部的恶性肿瘤,起源于鼻咽部上皮细胞。鼻咽癌的主要治疗策略是放疗加或不加化疗。大约7%至15%的患者在根治性放疗后仍有病灶残存或复发,10%至40%的患者在初次治疗后1至2年内复发。目前,对复发性鼻咽癌的管理还没有一个标准的治疗策略。手术是治疗复发性局部鼻咽癌的首选方法。调强放疗(IMRT)可以选择作为不可切除患者的一种挽救方式。近期,国内团队开展meta分析,评估复发性鼻咽癌挽救性手术治疗的效果。相关结果发表在Frontiers in Oncology杂志上。
最后筛选出21篇文章,其中17篇样本量大于10,纳入meta分析。10篇文章提供了详细的生存数据。
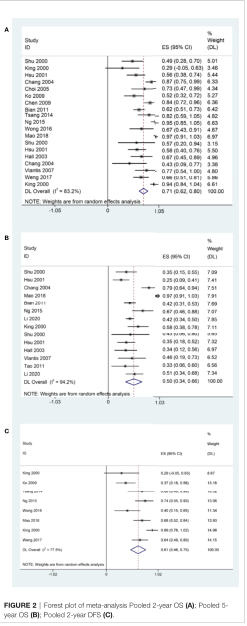
rNPC患者手术后联合或不联合辅助治疗的2年OS、5年OS和2年DFS为 71% (95% CI, 62%-80%, I 2 = 83.2%, p<0.05), 50% (95% CI, 34%-66%, I 2 = 94%, p<0.05)和61% (95% CI, 46%-75%, I 2 = 77.5%, p<0.05)。
手术治疗预后
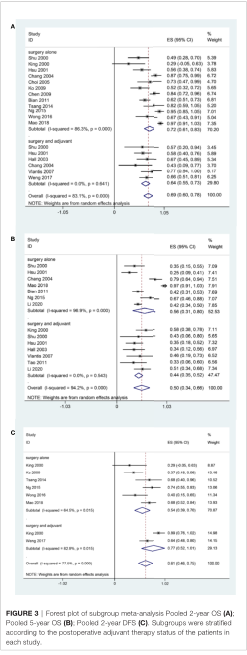
在亚组分析中,单独接受手术的患者2年OS率(72%,95% CI, 61%-83%, I 2 = 86.3%, p <0.05)比手术+辅助治疗患者的要好(64%,95% CI, 55%-73%, I 2 = 0.00%, p = 0.641)。术后辅助治疗组的5年OS率为44% (95% CI, 35%-52%, I 2 = 0.00%, p = 0.543), 单独手术治疗组为56% (95% CI, 31%-80%, I 2 = 96.9%, p<0.05)。术后辅助治疗组2年DFS为77% (95% CI, 52%-1.01%, I 2 = 77.5%, p<0.05),高于单纯手术组(54%,95% CI, 39%-70%, I 2 = 64.5%, p <0.05)。
亚组分析
研究进一步比较了单纯手术治疗的患者,开放手术组的5年OS为77.0%,内镜手术组为82.5% (p>0.05);开放手术组2年DFS为85.0%,内镜手术组2年DFS为72.5% (p >0.05)。对于开放手术治疗患者,术后辅助治疗患者的5年OS率为35.2%,单纯手术组为77.0% (p>0.05);而2年DFS率分别为37.3%和85.0% (p < 0.05)。对于内镜手术治疗患者,术后辅助治疗患者的2年OS率为67.3%,单纯手术治疗患者的为82.5%(p,0.05)。
切缘状态、复发T期、辅助治疗影响患者的生存预后。在单变量中被认为有意义的变量被纳入Cox多变量分析。Cox多因素分析中,复发T期和辅助治疗是鼻咽癌复发DFS的独立危险因素。
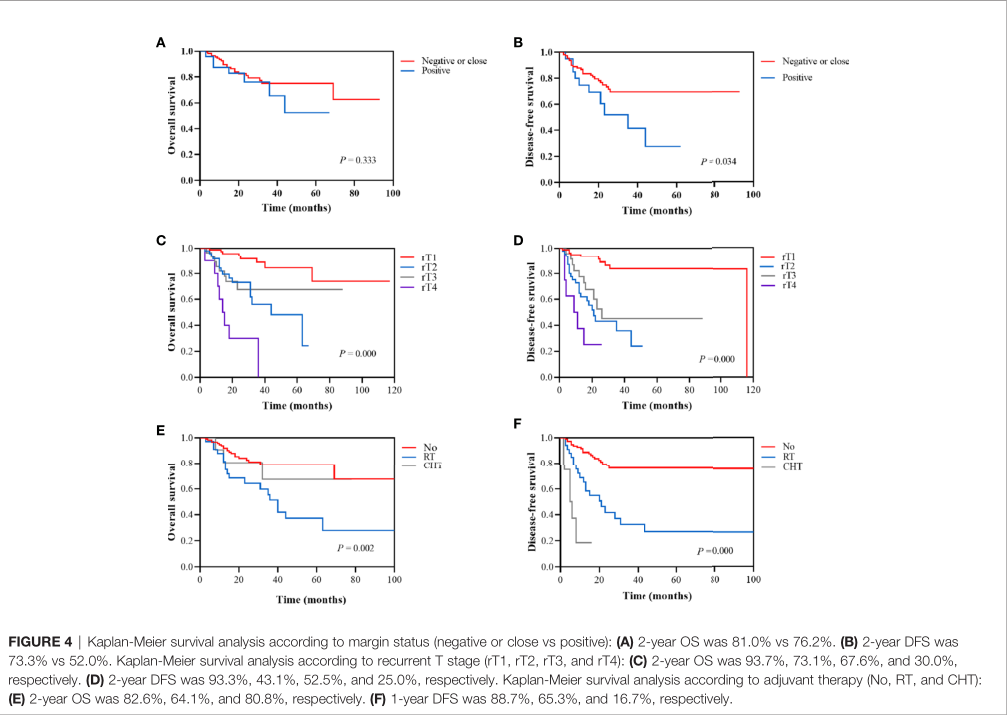
预后相关因素
综上,该荟萃分析表明,复发鼻咽癌患者挽救性手术有利于生存。准确评估肿瘤的复发分期和选择合适手术方式是成功关键。后期需要更多的随机对照研究去进一步证实。
原始出处:
Feng Y, Dai Z, Yan R, Li F, Zhong X, Ye H, Chen C, Fan S, Qing C, Pan Y and Sun H (2021) Outcomes of Recurrent Nasopharyngeal Carcinoma Patients Treated With Salvage Surgery: A Meta-Analysis. Front. Oncol. 11:720418. doi: 10.3389/fonc.2021.720418
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Meta#
21
#Oncol#
21
#MET#
24
#手术治疗#
30