Cell Research:邓宏魁课题组与罗佗平课题组报道特异性清除衰老细胞的新型化合物
2020-04-29 邓宏魁 生命科学联合中心
2020 年 4 月 27 日,生命科学联合中心邓宏魁课题组与罗佗平课题组合作,在《Cell Research》杂志在线发表了题为 “Elimination of senescent cells by
2020 年 4 月 27 日,生命科学联合中心邓宏魁课题组与罗佗平课题组合作,在《Cell Research》杂志在线发表了题为 “Elimination of senescent cells by β-galactosidase-targeted prodrug attenuates inflammation and restores physical function in aged mice” 的研究论文。该研究组针对衰老细胞的重要特征,巧妙设计并合成了一个新型化合物,证明了该化合物能够高效清除衰老个体中多个组织器官累积的衰老细胞,显着改善老年小鼠的生理状态,恢复老年小鼠的机体功能。
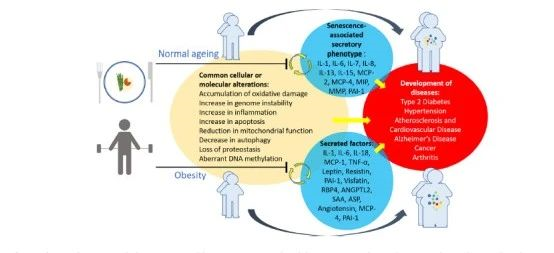
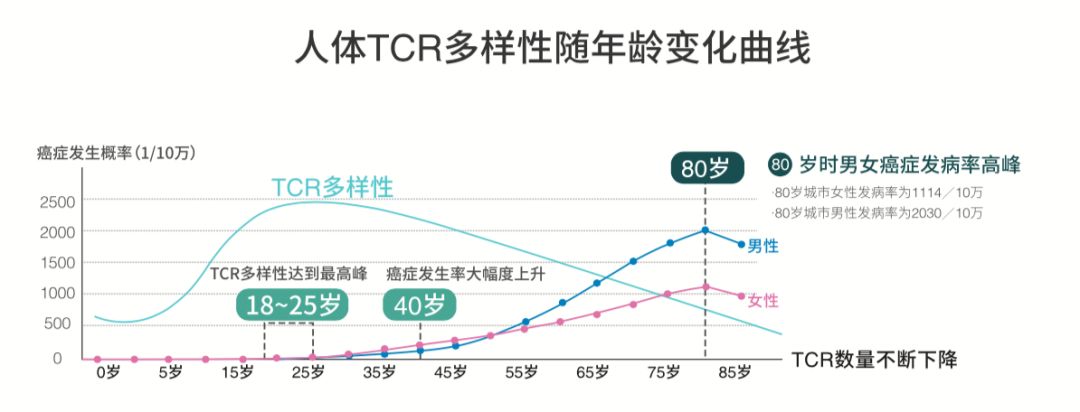
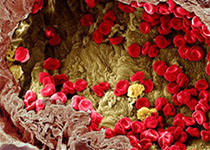
个体衰老伴随着机体各种生物学功能的逐渐衰退,其中一个重要特征是衰老细胞(senescent cells)在体内的累积。衰老细胞自身的功能失调,并分泌多种炎症因子和细胞因子,会造成组织器官功能紊乱并加速衰老进程。因此选择性清除体内衰老细胞成为抗衰老研究的重要方向。已报道的清除衰老细胞的化合物主要通过抑制细胞抗凋亡通路,诱导衰老细胞死亡。但这类化合物存在明显的局限性:其一,广谱性不强,不同类型衰老细胞激活不同的抗凋亡通路,所以靶向特定抗凋亡通路的小分子,无法有效清除体内多种类型的衰老细胞;其二,特异性不高,这类化合物在激活衰老细胞凋亡信号通路的同时,也会 “误杀” 非衰老细胞。因此,如何特异性清除体内多种组织器官累积的衰老细胞是一个关键的难题。
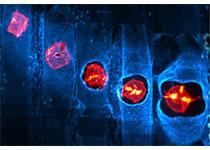
该项工作中,邓宏魁课题组与罗佗平课题组合作,建立了一个新的靶向清除衰老细胞策略。该策略利用衰老细胞普遍具有的最典型特征——增强的溶酶体β- 半乳糖苷酶(β-gal)活性,设计并合成了一个可以特异地被衰老细胞β- 半乳糖苷酶(senescence associated β-gal, SA-β-gal)代谢激活的新型抗衰老化合物——SSK1(senescence specific killing compound 1)。SSK1 本身不具有杀伤作用,当其进入衰老细胞,SSK1 的β- 半乳糖苷键会迅速被 SA-β-gal 切割, 释放具有杀伤性的毒性分子,诱导衰老细胞死亡;当 SSK1 进入非衰老细胞,由于β-gal 的活性较低,SSK1 不会被代谢激活,不会产生杀伤作用。研究组首先通过体外细胞实验,证实了 SSK1 高效清除多种类型的衰老细胞而不影响正常细胞存活,显示了该新型小分子化合物清除衰老细胞的广谱性和特异性。
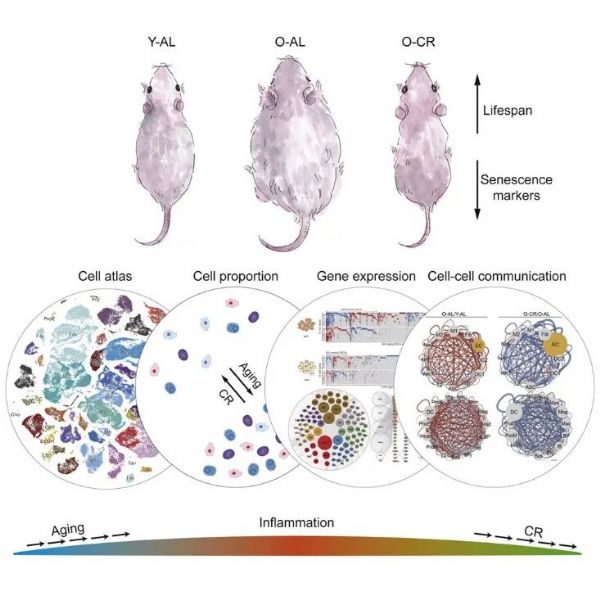
研究组进一步在体内验证了该新型小分子化合物清除衰老细胞与抗衰老的效果。首先,SSK1 可以显着降低衰老小鼠多个组织器官中衰老细胞的数量,逆转衰老相关的基因表达谱;其次,SSK1 显着减少组织及血液系统中衰老细胞分泌的多种炎症因子和细胞因子(senescence-associated secret phenotypes, SASP),缓解衰老相关的慢性炎症;进一步系统的功能学检测发现,经过 SSK1 处理后的老年小鼠,多种衰老相关的功能退化(运动耐力降低、肌肉力量减小、平衡能力变差和自发探索减弱)都得到明显改善,效果显着优于已报道的清除衰老细胞的化合物。研究组也对 SSK1 体内的安全性进行了系统检测,发现即使高剂量的 SSK1 也没有明显的毒副作用。
该研究工作首次证明了针对衰老细胞β- 半乳糖苷酶设计新一代小分子化合物 SSK1 清除衰老细胞的特异性和广谱性,该化合物能够有效减缓老年小鼠的衰老症状,显着改善老年小鼠的生理功能,为抗衰老药物研发提供了新的途径。
博士生蔡雨生、周欢欢和朱银华博士为本论文的共同第一作者;邓宏魁和罗佗平为论文的共同通讯作者;李程教授和博士生王龙腾也参与了这项工作。该工作得到了国家自然科学基金、国家重点研发计划、以及生命科学联合中心的资助。
原始出处:
Cai, Y., Zhou, H., Zhu, Y. et al. Elimination of senescent cells by β-galactosidase-targeted prodrug attenuates inflammation and restores physical function in aged mice. Cell Res (2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#特异性#
21
#CEL#
20
#Cell#
17
#化合物#
22
#Research#
20