European Radiology:使用深度学习从膝关节x线片进行骨龄评估
2022-06-09 shaosai MedSci原创
临床上提出了各种放射学方法来估计骨龄,从手、肘、膝、骨盆或脚的X光片,牙齿、锁骨或肋骨的计算机断层扫描(CT)到膝、手或髂嵴的磁共振成像(MRI)。
 通过放射学方法进行的年龄估计是通过评估扫描中的骨骼成熟度进行的,并在许多不同的情况下得到应用。在法医学中,其目的是确定未知死者的年龄,而在法律应用中,其目的是确定一个出生日期可疑的青少年是否达到法定年龄。在儿科内分泌学中,骨龄估计通常被用来确定是否存在生长障碍。
通过放射学方法进行的年龄估计是通过评估扫描中的骨骼成熟度进行的,并在许多不同的情况下得到应用。在法医学中,其目的是确定未知死者的年龄,而在法律应用中,其目的是确定一个出生日期可疑的青少年是否达到法定年龄。在儿科内分泌学中,骨龄估计通常被用来确定是否存在生长障碍。
临床上提出了各种放射学方法来估计骨龄,从手、肘、膝、骨盆或脚的X光片,牙齿、锁骨或肋骨的计算机断层扫描(CT)到膝、手或髂嵴的磁共振成像(MRI)。毫无疑问,从左手的X光片上估计骨龄是迄今为止临床上最常用的方法,但这种方法有一定的局限性。另一种估计骨龄的方法是基于膝关节的X光片。膝关节很适合于年龄估计,原因有以下几点。首先,膝关节可以提供三个骨骺(股骨远端、胫骨近端和腓骨近端)的信息;其次,膝关节扫描定位更便捷,而且辐射量很低;最后,由于膝关节在日常临床实践中经常被检查出有外伤,因此很容易建立大型的膝关节X光片系列。
现阶段,基于人工神经网络的深度学习方法已被用于基于手部X光片的年龄自动化评估,还没有类似的基于膝关节X光片的年龄自动化评估。近日,发表在European Radiology杂志的一项研究应用深度学习方法来证明膝关节X光片年龄自动化评估的可行性,为满足人们对骨龄评估的准确性及便捷性要求提供了技术支持。
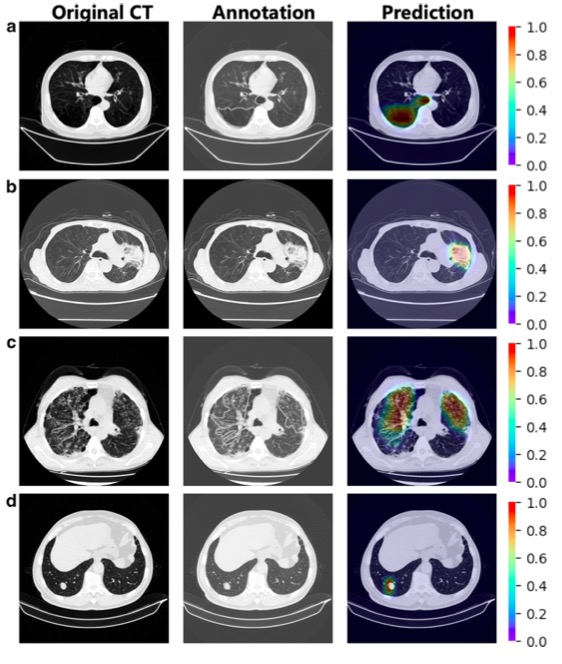
本项回顾性研究收集了3816张儿科患者的膝关节X光片(在2008年1月至2018年12月期间获得)对一个神经网络进行了训练。该网络被训练为从膝关节X光片中预测年龄,并在423张X光片的独立验证队列(2019年1月至2020年12月期间获得)和197张X光片的外部验证队列上进行了评估。
该模型在内部和外部验证队列中显示的平均绝对误差分别为0.86±0.72岁和0.9±0.71岁。年龄段区分(<14岁与≥14岁,<18岁与≥18岁)显示AUCs在0.94和0.98之间。
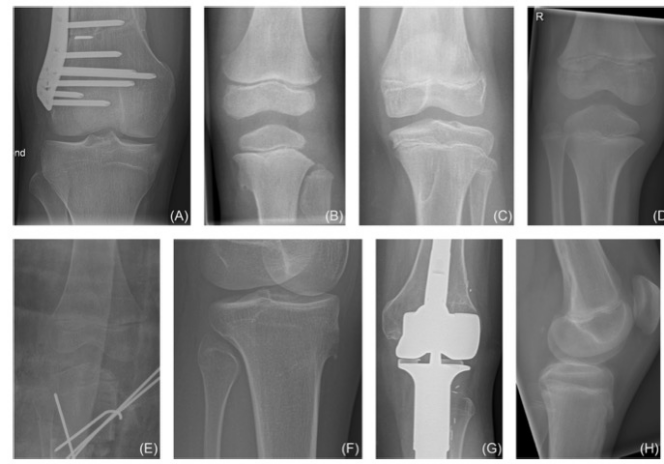
图 上行描述的是被纳入研究的X光片,下行是被排除的X光片示例。A 男性患者(18.5岁)。B 女性患者(3.3岁)。C 女性患者(13.0岁)。D 男性患者(6.8岁)。E 女性患者(15.7岁),因图像质量低而被排除。F 女性患者(5.3岁),因膝关节不完全可见而被排除。G 女性患者(19.8岁),因膝关节置换术被排除。H 男性患者(16.5岁),因为侧位图而被排除
本研究表明,使用深度神经网络可以从膝关节X光片中高度准确地评估出儿科病人的年龄,这为进一步的儿童骨龄评估提供了有价值的参考。
原文出处:
Aydin Demircioğlu,Anton S Quinsten,Michael Forsting,et al.Pediatric age estimation from radiographs of the knee using deep learning.DOI:10.1007/s00330-022-08582-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
55
高峰值
49
#X线#
42
#X线片#
56