Nat Commun:SWI/SNF复合物的具体组成在前列腺癌谱系可塑性中的作用
2020-11-22 AlexYang MedSci原创
晚期前列腺癌最初对激素治疗有响应,但最终会产生耐药性,从而需要更有效的治疗方法。研究人员在这些患者的10%-20%的比例中观察到的耐药性机制之一是谱系可塑性,表现为部分或完全的小细胞或神经内分泌前列腺
晚期前列腺癌最初对激素治疗有响应,但最终会产生耐药性,从而需要更有效的治疗方法。研究人员在这些患者的10%-20%的比例中观察到的耐药性机制之一是谱系可塑性,表现为部分或完全的小细胞或神经内分泌前列腺癌(NEPC)表型。
最近,有研究人员调查了哺乳动物SWI/SNF(mSWI/SNF)染色质重塑复合物在NEPC中的作用。研究人员使用了大型患者数据集,患者来源的器官和癌症细胞系,确定了在NEPC中失调的mSWI/SNF亚基,并阐释了SMARCA4(BRG1)的过表达与侵袭性疾病相关。研究人员还表明,与前列腺癌相比,SWI/SNF复合物在NEPC中与不同的谱系特异性因子相互作用。
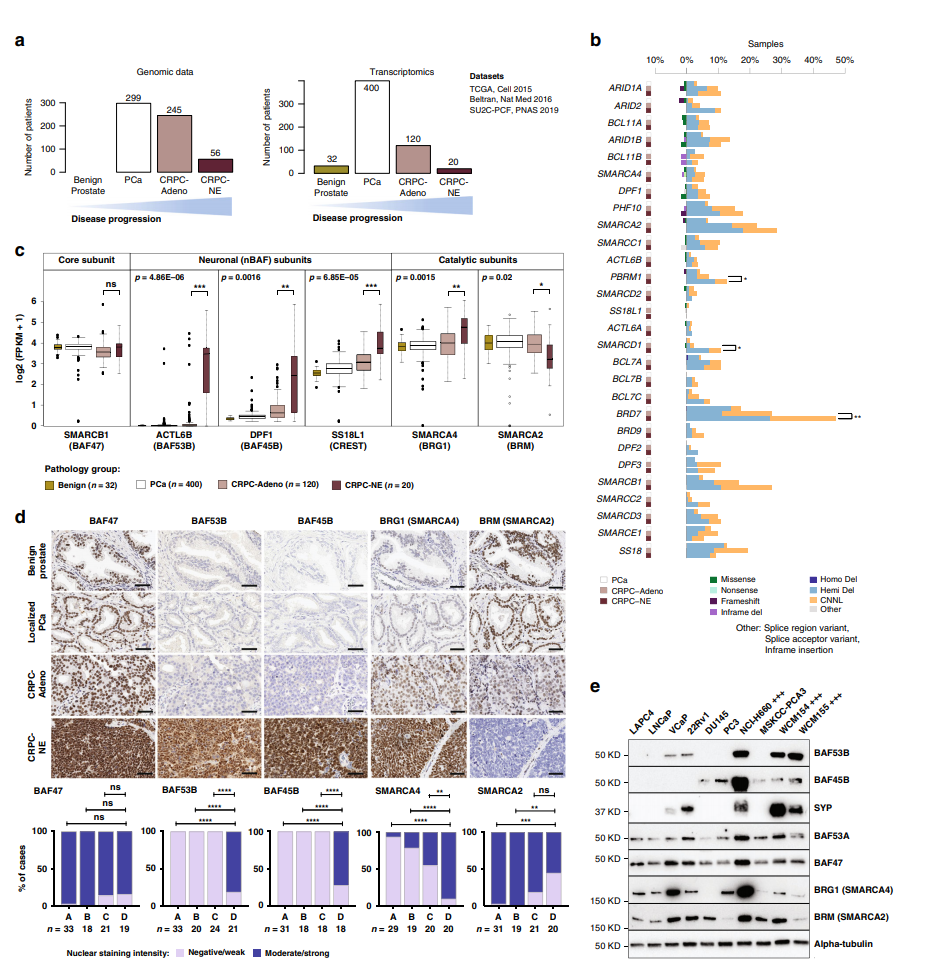
CPRC-NE中SWI SNF亚单元异常调节
这些数据指出了mSWI/SNF复合物在治疗相关谱系可塑性中的作用,这也可能与其他实体瘤相关。
原始出处:
Joanna Cyrta, Anke Augspach, Maria Rosaria De Filippo et al. Role of specialized composition of SWI/SNF complexes in prostate cancer lineage plasticity. Nat Commun. Nov 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#复合物#
45
#COMMUN#
38
#Nat#
37
前列腺癌相关研究,学习了,谢谢梅斯
59
学习学习
83