祝之明:难治性内分泌高血压的微创消融治疗
2021-01-31 《门诊》杂志 门诊新视野
美国心脏协会(AHA)难治性高血压专家共识指出,继发性高血压是难治性高血压的主要原因之一,而在继发性高血压中,内分泌性疾病特别是肾上腺疾病引起的高血压占据相当大的比重。
2018年美国心脏协会(AHA)难治性高血压专家共识指出,继发性高血压是难治性高血压的主要原因之一[1],而在继发性高血压中,内分泌性疾病特别是肾上腺疾病引起的高血压占据相当大的比重。近年来,针对难治性高血压,除了生活方式干预和药物治疗外,器械治疗尤其是肾动脉去交感神经消融术(RDN)得到了高血压治疗领域广大临床医师越来越多的重视和关注。然而,RDN的主要适应症为难治性原发性高血压,针对继发性高血压特别是内分泌性疾病引起的难治性高血压,除了外科手术外,是否也有相应的器械治疗方法,相关研究报道较少。
难治性内分泌高血压治疗的局限性
在难治性高血压中,肾上腺源性高血压占据主要部分,其中主要包括原发性醛固酮增多症(原醛症)、儿茶酚胺增多症、皮质醇增多症,这部分患者往往伴随持续性血压升高且难以控制,给患者带来的心血管风险较大。但目前针对这部分患者的治疗手段存在一定局限性。
药物治疗存在的局限性主要在于,采用醛固酮受体(MR)拮抗剂并未能有效降低原醛症患者的心血管风险。2018年哈佛大学发表的一项回顾性分析显示,与年龄匹配及血压水平相似的原发性高血压患者相比,MR拮抗剂治疗的原醛症患者,如果肾素仍然受到抑制,其发生心血管事件(心肌梗死,卒中,因心力衰竭住院)的风险几乎高出3倍[2]。此外,过度使用该药物则可带来副作用的明显增加,包括男性乳房增生、女性月经不调及其它一些中枢神经系统副作用等。
相比于药物治疗,手术治疗可带来更多获益。有研究显示,与药物治疗相比,从长期来看手术治疗可显着降低原醛症患者醛固酮分泌水平,而药物治疗(如螺内酯)并未能有效降低患者的醛固酮水平[3-4]。
然而,手术治疗(肾上腺切除术)的优缺点并存。肾上腺切除术的优点较多,特别是对于醛固酮腺瘤患者的疗效确切,50%患者高血压可治愈,94%患者血钾与醛固酮可恢复至正常水平,且术后有病理学佐证。但该手术最大难点在于术前需行肾上腺静脉取血(AVS)以确定优势分泌侧,而国内目前可行AVS的医院大概仅1%左右,如未行AVS,仅依据CT结果,可能导致误诊;且术后具有肾上腺功能低下风险,后期处理困难。
也有研究显示,肾上腺切除术降压效果有限。一项荟萃分析显示,肾上腺切除术后血压控制率仅为52%,且术后血压控制正常比例将按照6.7%/年的比例逐年降低[5];另一项纳入全球10个国家28个中心的研究显示,肾上腺切除患者(n=705)血压完全控制率仅37%,血压部分缓解率仅47%[6]。因此,尽管目前手术治疗可带来比药物治疗更好效果,但疗效有限,探索其它新的手术治疗方式势在必行。
难治性内分泌高血压治疗的消融治疗
消融治疗的适应症包括:药物治疗效果欠佳,不能耐受药物副作用,且无外科手术适应症者;有手术指征,但不愿行外科手术或手术风险大者;外科手术后疗效不佳,经药物治疗疗效欠佳者;依据AVS明确存在高分泌(有或无瘤体)侧者。
消融治疗主要包括两种:
一种是物理消融,比如CT引导经皮射频物理消融术。射频物理消融(RAF)的基本原理是利用射频治疗仪产生热效应造成细胞死亡和溶解,减少肾上腺多种激素的分泌,从而降低血压;
另一种是化学消融,比如超选肾上腺动脉化学消融术。采取上肢桡动脉路径送入微导管,无水乙醇用作栓塞剂,可引起肾上腺组织蛋白凝固性坏死,减少肾上腺多种激素的分泌,从而降低血压。
近年来,大坪医院针对非腺瘤型原醛症患者采用肾上腺消融治疗也取得了较理想治疗效果。经消融治疗后,9例患者(25%)达到血压完全缓解(血压下降20 mmHg/16 mmHg),13例患者(36%)达到部分缓解(血压下降30 mmHg和14 mmHg),治疗后血压较术前明显改善比例达61%;术后血钾、ARR恢复正常患者比例达44.4%。在安全性方面,患者未出现肾上腺皮质功能低下症状,主要副作用为部分患者出现消化道症状(如恶心、呕吐)、腰背部疼痛,但对症治疗数天后恢复[7]。此外,大坪医院针对腺瘤术后复发患者进行消融手术,也获得了类似效果,包括血压下降30 mmHg/10 mmHg,且术后ARR恢复至正常范围(<20)[7]。
与主要适应症为难治性原发性高血压的RDN相比,肾上腺消融术主要适应症为继发性高血压(如原醛症和皮质醇增多症等),疗效评价指标为特异性激素水平变化,术后25%患者可停药,副作用相对较少,且小样本病例提示其长期疗效明确。(表1)
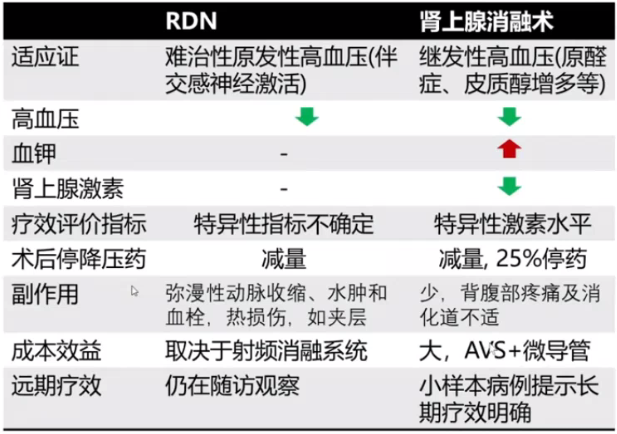
表1. 去肾交感神经消融术(RDN)与肾上腺消融术对比
经典病例分享
报告中,祝之明教授详细阐述了3例采用肾上腺消融术的经典病例,因篇幅受限,下列举其中一例。
患者,男,49岁,血压高15年,血压波动大1月;
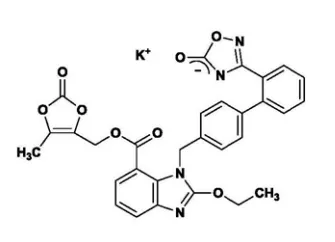
现病史:高血压15年,140/100 mmHg,长期予以“吲达帕胺”降压治疗。1年前因血压控制不佳,调整降压药物为“硝苯地平控释片、氯沙坦钾氢氯噻嗪片、富马酸比索洛尔片”。1月前测血压波动较大,波动在140~170/90~100 mmHg,伴夜尿频,于2016-09-09我科诊治;
RAAS激素(放免法):立位:醛固酮0.2 ng/ml,肾素0.45 ng/ml.h,血管紧张素Ⅱ 63 pg/ml,ARR 44;卧位:醛固酮0.17 ng/ml,肾素0.41 ng/ml.h,血管紧张素Ⅱ 69 pg/ml,ARR 41;皮质醇节律及ACTH节律、肝肾功无明显异常;
生化指标:血钾2.98 mmol/L;尿钾:57.43 mmol/24h;
动态血压:平均血压,白天149/85 mmHg,夜间134/76 mmHg,全天136/83 mmHg,平均心率75次/分;
靶器官相关检查情况。心电图提示:窦性心动过缓;心脏超声提示:左房增大,室间隔增厚,左室舒张功能减退;颈动脉超声提示:右侧颈动脉斑块形成,左侧颈动脉窦部增宽;腹部超声提示:脂肪肝;24小时尿微量白蛋白及总蛋白无明显异常;
肾上腺CT影像:双侧肾上腺增生,右侧肾上腺内支结节性增生;(图1)
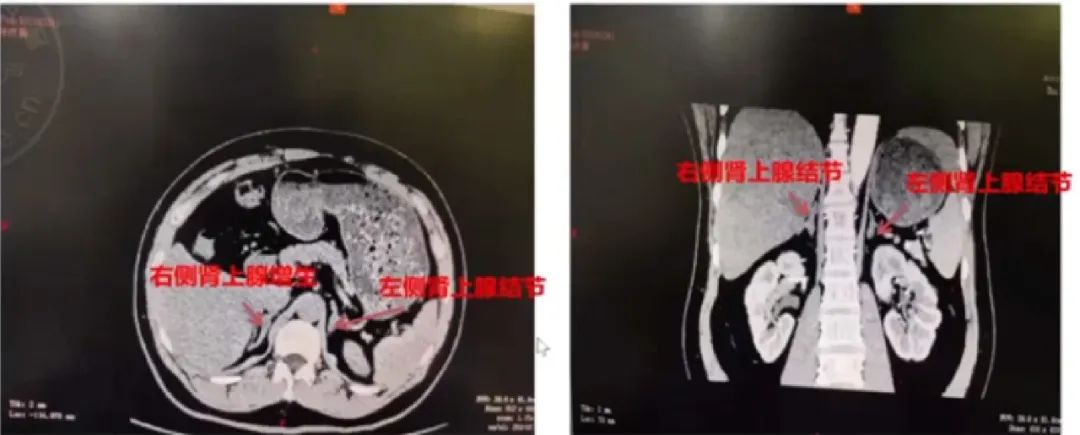
图1. 肾上腺CT影像结果
原醛症的确诊与分型(表2)
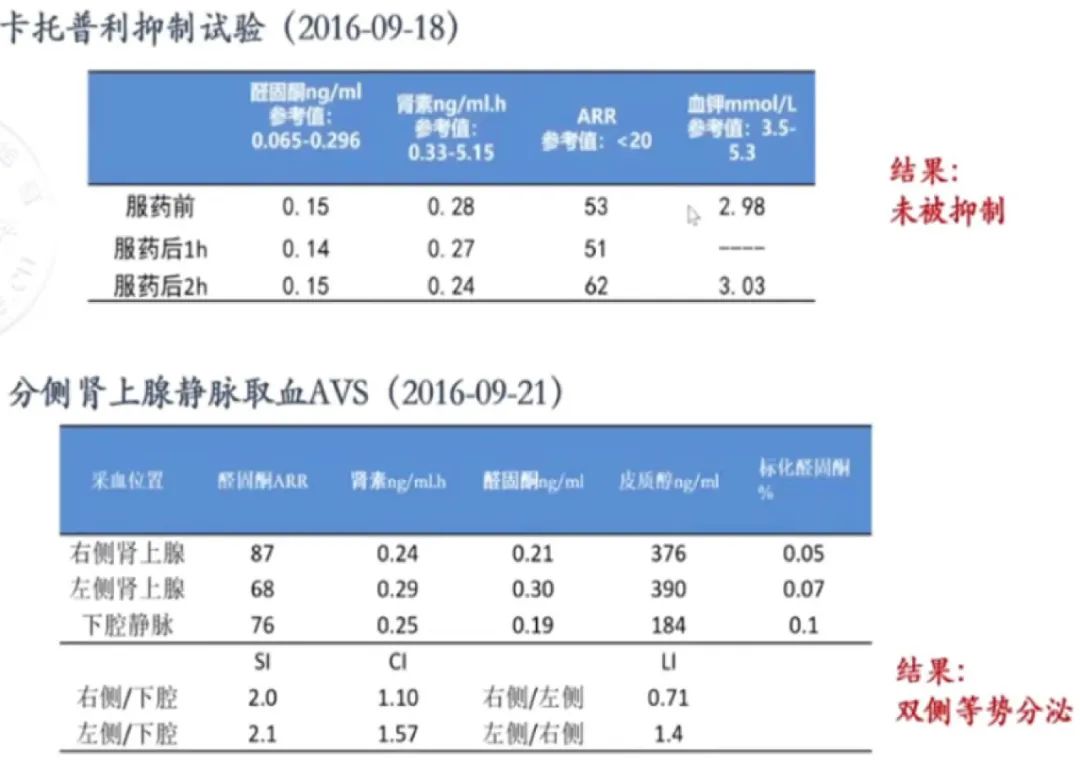
表2. 原醛症的确诊与分型
出院诊断:原发性醛固酮增多症(双侧肾上腺增生);
治疗方案:药物治疗(苯磺酸氨氯地平片5 mg 2/日+螺内酯片20 mg 3/日);经治疗后血压控制尚可,但服用螺内酯后逐渐出现双侧乳腺发育伴刺痛;
再次入院的基本情况
现病史:患者于2016-09-23自我院出院后,院外口服“螺内酯片”出现乳房刺痛及增生等不适后自行减量螺内酯,但血压波动较大且反复低血钾,于我科门诊再次就诊。为进一步诊治于2019-03-07再次入院;
现用药史:苯磺酸氨氯地平片5 mg 1/日,盐酸特拉唑嗪片2 mg 1/日;
RAAS激素:立位醛固酮362 pg/ml,肾素0.54 ulU/mL,ARR 670;
生化指标:血钾3.37 mmol/L;尿钾:45.47 mmol/24h;
肾上腺CT:双侧肾上腺增生,左侧肾上腺内支结节影,与2016年09月比较,未见明显变化;
动态血压:平均血压,白天149/85 mmHg,夜间134/76 mmHg,全天136/83 mmHg,平均心率75次/分;
内外科治疗方案:因药物副作用不能耐受,故选择放弃继续口服MR受体拮抗剂;另外,泌尿外科医师会诊认为该患者肾上腺形态只是增生,没有明显腺瘤,且AVS结果提示对侧肾上腺功能明显被抑制,担心术后出现肾上腺皮质功能低下风险,所以不建议行外科切除手术;
术后改善情况:通过对该患者行超选右侧肾上腺动脉消融术,术后患者醛固酮水平大幅下降,肾素水平升高,ARR大幅下降,血钾恢复正常,血压也得到很好控制,每天只需服用1片苯磺酸氨氯地平(5 mg)。(图2)
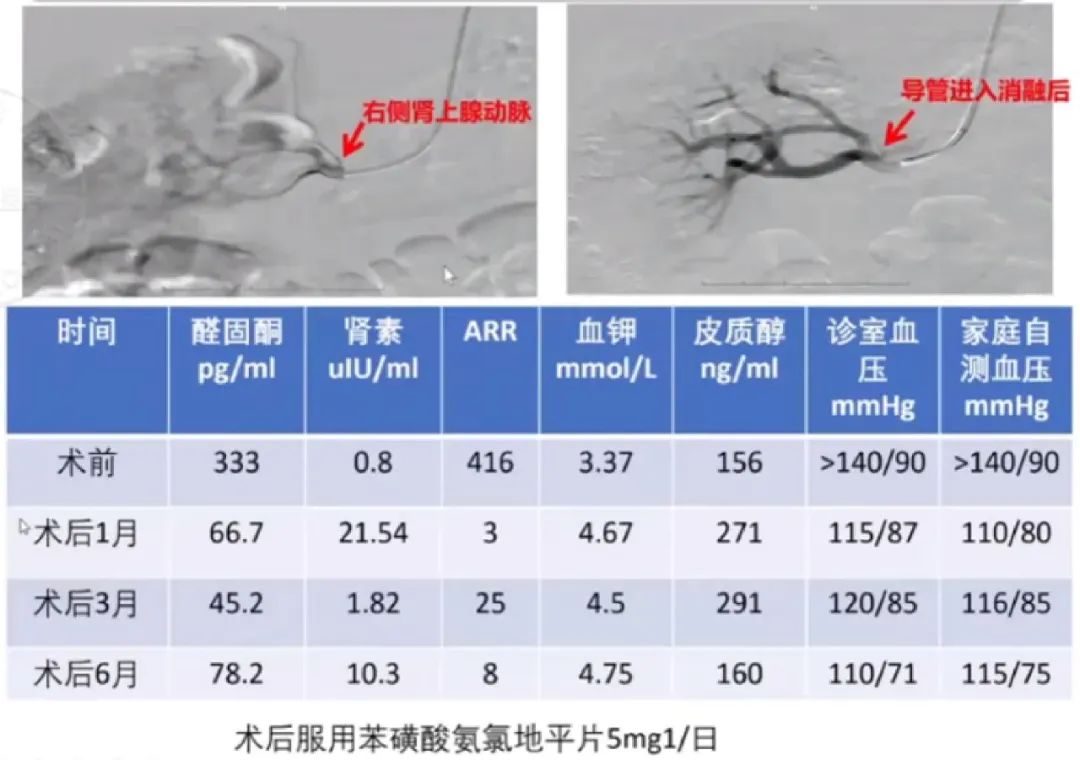
图2. 行肾上腺消融术后疗效
总 结
肾上腺性高血压,属于难治性高血压,有较大的心脑血管风险。针对非腺瘤且仅具一侧高分泌的肾上腺性高血压患者的诊断具有很大挑战性,合理运用AVS对肾上腺性高血压进行精准诊治十分重要。传统的药物治疗和外科手术治疗肾上腺性高血压均有一定的局限性,超选肾上腺动脉化学消融术是对传统治疗的重要补充,具有疗效确切,安全及副作用少的特点。内分泌评估与AVS是确定消融治疗的基础,消融失败可继续外科手术治疗,因此多学科协作是开展这项技术的重要保障。
原始出处:
[1] Hypertension. 2018;72:e53-e90.
[2] Lancet Diabetes Endocrinol. 2018;6:51.
[3] Hypertension. 2007;50:911-918.
[4] Hypertension. 2016;68:204-212.
[5] J Clin Hypertens. 2016;18:1205-1212.
[6] Lancet Diabetes Endocrinol. 2017 Sep;5(9):689-699.
[7] J Clin Hypertens (Greenwich). 2020 Sep;22(9):1618-1626.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#分泌#
51
#微创#
63
#消融#
55
#难治性#
57
#消融治疗#
59
11111111
88