EuroPCR2018:SPYRAL HTN-ON MED试验发布,经导管去肾交感神经术的又一里程碑式研究
2018-05-24 佚名 中国循环杂志
昨日,在欧洲心血管介入会议(EuroPCR)2018年年会上,SPYRAL HTN-ON MED试验再次为经导管去肾交感神经术(RDN)加了“一把火”,研究表明:RDN可有效治疗轻中度高血压。
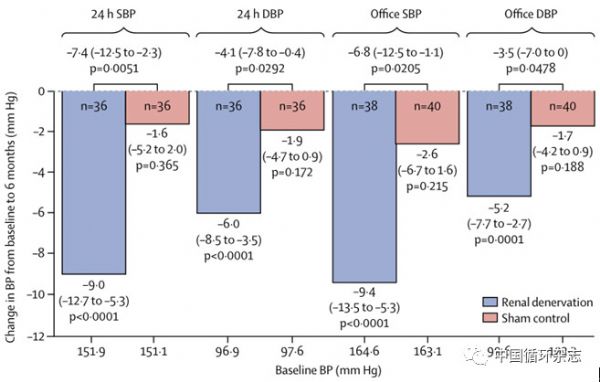
研究显示,接受RDN治疗的轻中度高血压患者,与假手术组相比,在随访6个月时,24小时平均收缩压和平均舒张压、诊室收缩压和舒张压均明显下降。
RDN组24小时平均收缩压下降了9 mm Hg,平均舒张压下降6 mm Hg,诊室收缩压下降了9.4 mm Hg,诊室舒张压降低了5.2 mm Hg;而假手术组24小时平均收缩压下降了1.6 mm Hg,平均舒张压下降了1.9 mm Hg,诊室收缩压下降了2.6 mm Hg,诊室舒张压降低了1.7 mm Hg(图1)。
研究还显示,在3~6个月的随访期间,随着时间推移血压下降程度逐渐增加,昼夜血压均有明显下降(图2)。
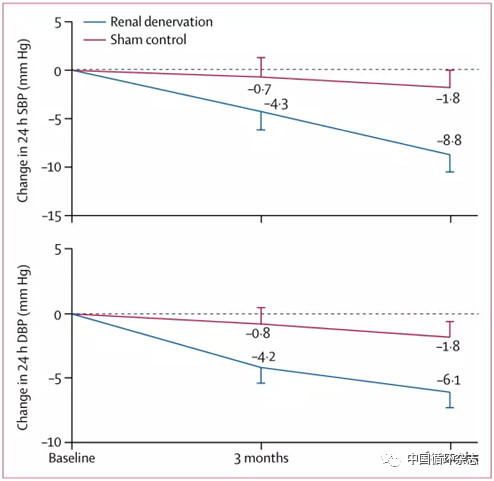
图2 接受经导管去肾交感神经术治疗组和假手术组随访3~6个月期间24h动态血压监测情况
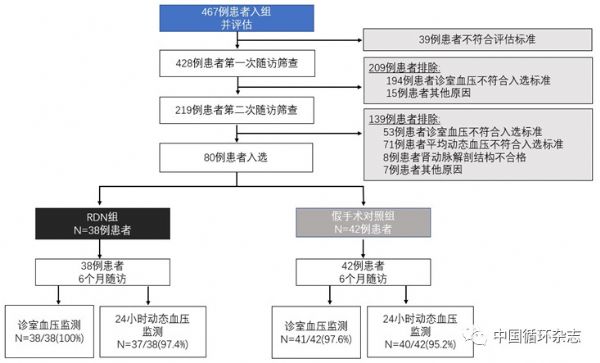
SPYRALHTN-ON MED试验最终共纳入80例患者,其中RDN治疗组38例,假手术对照组42例(图3)。入选标准:诊室收缩压≥150 mmHg且<180 mmHg,诊室舒张压≥90 mmHg,24小时平均收缩压≥140 mmHg且<170 mmHg。
试验排除了肾动脉解剖不适于导管消融治疗者、估算肾小球滤过率(eGFR)<45mL/(min·1.73m2)的严重肾病患者、1型糖尿病或HbA1C>8.0%者以及继发性高血压患者。
所有受试者,第一次筛查前降压药必须稳定服用至少6周,降压药包括噻嗪类利尿剂,二氢吡啶类钙拮抗剂以及血管紧张素转换酶抑制剂或血管紧张素受体拮抗剂等1~3种,且至少服用最大推荐剂量的50%。所有受试者在入组前和术后检测尿液来验证是否使用降压药。
RDN自2009年首次被报道治疗难治性高血压效果显着以来,受到了广泛关注,也因SYMPLICITY HTN-3研究受到质疑。那么,如何解读SPYRAL HTN-ON MED试验,认识RDN?
天津市第一中心医院卢成志教授从以下几个方面就此进行了剖析和点评。
点评专家简介:卢成志 教授 天津市第一中心医院 教授,国务院特贴专家,主任医师,博士生导师,硕士生导师 现任天津市第一中心医院心脏科主任,中华医学会天津心血管分会副主任委员,中国医师协会心血管分会委员,天津市医师协会心血管分会副会长,天津市自然科学基金项目评审专家。
SPYRAL HTN-ON MED试验:采用多电极消融导管
他指出,SPYRAL HTN-ON MED与SYMPLICITY HTN-3两项研究试验结果不同的原因是多方面的。
首先,SPYRAL HTN-ON MED试验对受试者筛选较为严格,最大特点是固定了受试者降压药使用类别,减少了混杂因素,并且更多地关注24小时平均动态血压。
其次,工欲利其事,必先利其器,合适的消融设备对消融设备是RDN成功的重要因素之一。SPYRAL HTN-ON MED研究采用的是第二代Symplicity Spyral?消融导管(美敦力),导管上有4个电极以90°的间隔均匀分布在螺旋型电极环的四个象限中,释放于肾动脉后可自动恢复螺旋形。
此导管可克服既往SYMPLICITY系列研究单电极导管的不足,可以多个位点同时消融,节约手术时间。同时消融位点相对固定,可以减少术者手术操作的差异。
第三,在手术操作方面,SPYRAL研究消融部位包括肾动脉主干及分支,而这能够起到更好的降压作用。
他也指出,SPYRAL HTN-ON MED试验也存在一定局限性,如试验设计没有包括预期统计功效评估;降压药的遵医嘱率较低,仅有60%。另外研究结果不一定代表其他RDN设备;没有适合指标判断消融是否成功。
SPYRAL HTN-ON MED试验对临床实践的影响:肾交感型高血压患者或获益最大
卢成志表示,近10年RDN安全性观察均证明RDN在手术操作及肾功能影响等各方面都是安全的。对于难治性高血压及轻中度高血压均有效。鉴于SPYRAL HTN ON-MED研究的有利结果,并结合既往研究,RDN仍是高血压治疗的一种可选,甚至是药物替代疗法,但是必须严格把控适应证,而且对于适于RDN治疗的高血压患者还需进一步研究来明确。
他认为,SPYRAL HTN-ON MED试验也不是一个终点,只是RDN发展中的又一里程碑,更大样本量的Pivotal研究,还需拭目以待。
就目前而言,肾交感型高血压患者,或许最大获益于RDN。此外,不合并或合并较少的靶器官损伤的年轻高血压患者,接受RDN治疗,或许能延迟高血压药物治疗或至少延缓高血压进程。
此外,对于动脉硬化度较低的收缩压和舒张压均升高的患者,RDN治疗效果也明显优于单纯收缩期高血压患者。
还有就是对于特殊类型的高血压患者,入院育龄期女性妊娠前接受RDN治疗,可能可以减少或替代降压药物使用。另外难以按时服药的轻中度高血压患者也可考虑此治疗。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#里程碑#
29
#去肾交感神经术#
39
#EuroPCR#
30
#里程碑式研究#
36
学习了谢谢分享!!
63
#PCR#
31
#经导管#
21
#Med#
26