肝癌是高发病率,高致死率的恶性疾病,全世界和中国的年新发病例数分别为90.6万和37.0万,年新增肝癌致死病例数分别高达83.0万和32.6万。肝细胞癌 (HCC) 是全世界最高发的肝癌类型,约占原发性肝癌总数的75.0%~90.0%。尽管近年来医疗技术和治疗方法有所改进,但HCC的5年生存率仍然很低。

pixabay
多项指南建议,通过筛查对高危人群进行早期检测有助于提高HCC的生存率。然而高危人群对定期筛查的依从性不足,导致超声检查整体效益降低。此外,在评估筛查项目时,研究人员也很少对HCC患者的生活质量和终生生存效益进行量化。
近日,发表在JAMA Netw Open杂志的一项研究探讨了对于HCC高危人群来说,超声检查的早期诊断最佳时间间隔。结果发现,6至12个月或更短的超声检查时间间隔,可能会对HCC的早期发现有着很大的帮助,并可能挽救更多的HCC患者的生命。
在这项研究中,研究人员使用来自台湾的三个数据库进行研究,包括台湾国民健康保险、台湾国家癌症登记处和国家死亡率登记处。对 2002 年至 2015 年新诊断为 HCC 的114022名患者进行了随访至 2017 年。根据患者最后一次超声检查的日期(HCC诊断前90天),将患者分类为5个时间段,分别为6个月(0-6个月),12个月(7-12个月),24个月(13-24个月),36个月(25-36个月),以及超过36个月(过去3年没有筛查)。数据分析时间为 2020 年 4 月至 2021 年 4 月。
研究结果显示,共收纳59194名患者,42081名男性,平均年龄为62.2岁和17113名女性,平年龄为69.0岁。超声检查的间隔时间越长,男女的预期寿命损失和质量调整生命年(QALY)失越高。对于 6 个月的超声筛查间隔,男性QALY值为10.0,间隔时间为12个月,QALY值为11.1,间隔时间为24 个月,QALY值为12.1, 间隔时间为36 个月,QALY值为13.1, 间隔时间超过36个月,QALYs 值为14.6。
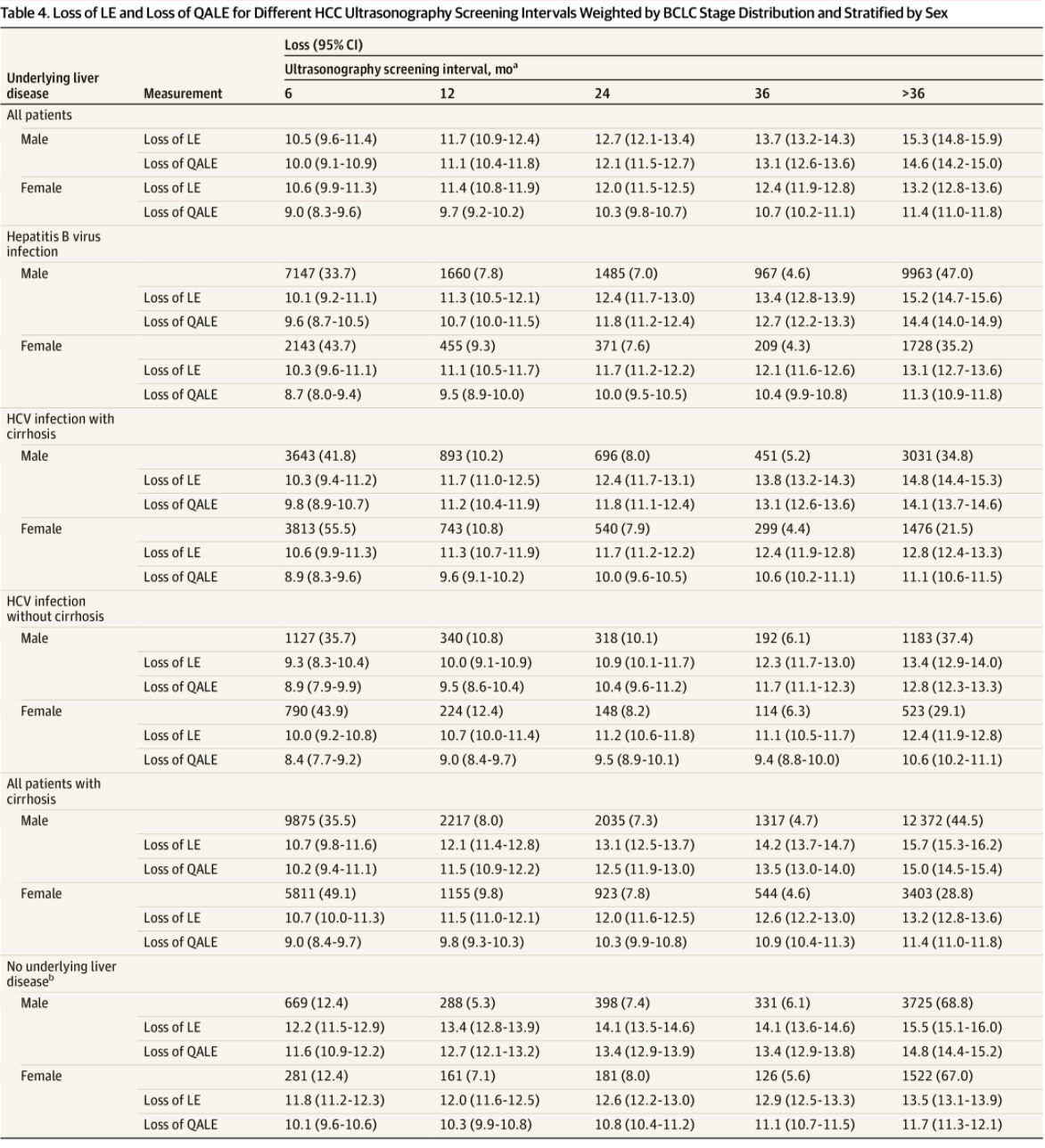
按性别分层的不同 HCC 超声筛查间隔与QALY损失
在女性中, 6 个月的超声筛查间隔,QALY值为9.0,间隔时间为12个月,QALY值为9.7,间隔时间为24 个月,QALY值为10.3, 间隔时间为36 个月,QALY值为10.7, 间隔时间超过36个月,QALYs 值为11.4。另外,有潜在乙型肝炎病毒感染或肝硬化的患者在较短的筛查间隔期内预期寿命的改善最大。
综上,这项研究的结果表明,间隔 6 至 12 个月或更短的定期超声检查可能有助于HCC 的早期检测,并可能挽救更多生命。另外,观察到,有乙型肝炎病毒或丙型肝炎病毒感染、肝硬化和酒精性肝病等人群显示出更频繁的超声检查。
原始出处
Shih-Chiang Kuo, MD1; Chia-Ni Lin, RN, MS2; Yih-Jyh Lin, MD1,3; et al.Optimal Intervals of Ultrasonography Screening for Early Diagnosis of Hepatocellular Carcinoma in Taiwan.JAMA Netw Open. 2021;4(6):e2114680. doi:10.1001/jamanetworkopen.2021.14680
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#NET#
27
#肝细胞#
32
#细胞癌#
26
#PE#
39
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
47