Movement Disordres-帕金森病患者血浆中糖磷脂的变化与葡萄糖酰甘油水平无关
2022-08-18 Freeeman MedSci原创
在有和没有GlcCer变化的患者中检测到血浆中多种GSL异常,表明脂质平衡有更广泛的转变。
帕金森病(PD)是全球第二大最常见的神经退行性疾病。脂质改变,特别是糖磷脂(GSLs)的变化,最近在PD发病机制中获得了关注。编码葡萄糖酰甘油酰胺(GlcCer)降解酶(GCase)的GBA杂合子突变被确定为PD最常见的遗传风险因素,这就突出了脂质的作用。GBA1突变携带者增加PD风险的机制尚不完全清楚。
图1: 论文封面图
在有和没有GBA1突变的PD患者的脑组织中,以及在健康的老龄化受试者中,已经描述了GCase活性的降低,但最近的一项研究显示GCase总活性和PD风险之间没有相关性。总之,GSL在散发性PD中的作用,独立于GBA1相关疾病,需要更广泛的检查和进一步的澄清。
藉此,牛津大学的Danielle te Vruchte等人,分析了与健康对照组(HC)相比,PD受试者血浆中GSLs的水平。他们发现大多数PD血浆样本中GlcCer增加,因此,他们进一步对PD人群进行分层,评估其他GSL的变化是否受到高GlcCer水平的影响,因为GlcCer是所有GSL的前体。此外,作为一个探索性结果,我们分析了特定的GSLs是否与临床特征相关。
他们用两种正相高效液相色谱法分析血浆中的GSLs和葡糖甘油酰胺(GlcCer);提取临床人口学数据。
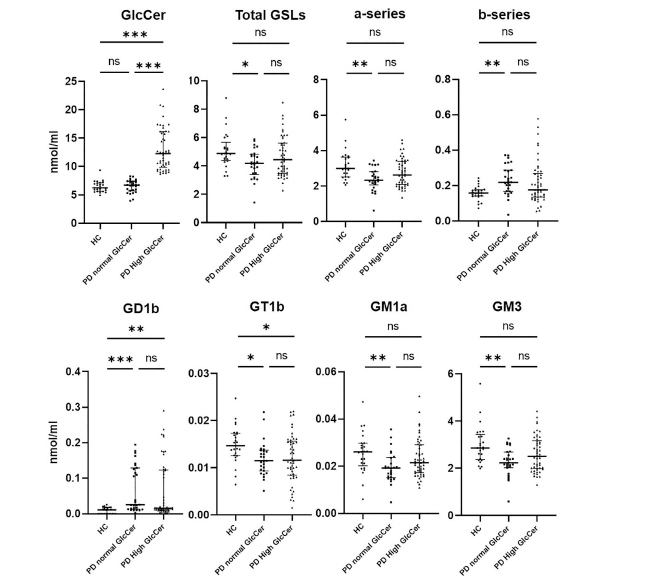
图2:论文结果图
他们分析了80名PD受试者和25名HCs。
PD患者的GlcCer、GD1b、Gb4、GalNAcGA1和b系列的水平高于HCs;PD患者的总GSLs、GT1b、GM1a、GM3、GM2和a系列水平低于HCs。在PD受试者中存在GSLs的变化,GlcCer水平与HCs的水平相似。
在排除某些GBA1突变携带者后,结果相似。运动障碍协会统一帕金森病评分表第三部分与Gb4相关,蒙特利尔认知评估与GD1b水平相关。
该研究的重要意义在于发现了:在有和没有GlcCer变化的患者中检测到血浆中多种GSL异常,表明脂质平衡有更广泛的转变。
原文出处:
te Vruchte D, Sturchio A, Priestman DA, et al. Glycosphingolipid Changes in Plasma in Parkinson’s Disease Independent of Glucosylceramide Levels. _Movement Disorders_. Published online July 25, 2022:mds.29163. doi:[10.1002/mds.29163](https://doi.org/10.1002/mds.29163)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#帕金森病患者#
36
#Dis#
31
#Disord#
46
#期刊论坛##学习#
0
不错的文章
47
好文章,谢谢分享。
28
#帕金森病患#
46