Eur J Cancer:可准确评估局部晚期乳腺癌患者NAC后的完全缓解的深度学习模型!
2021-02-25 MedSci原创 MedSci原创
局部晚期乳腺癌新辅助化疗后是否获得完全缓解?
局部晚期乳腺癌(LABC)常采用新辅助化疗(NAC)。NAC可以在手术前安全地缩小肿瘤体积,可为原本丧失手术机会的患者重新获得手术切除肿瘤的机会。
本研究旨在开发并验证一种基于治疗前后超声检查的深度学习放射线诺模图(DLRN),用于术前评估NAC后乳腺癌的病理完全缓解(pCR)情况。
从两家医院招募了拟进行术前NAC的组织学明确的LABC患者(训练队列,n=356;独立外部验证队列,n=236)。提取可反映治疗前(放射学特征[RS] 1)和治疗后肿瘤(RS2)表型的深度学习和手动放射特征。最小冗余最大相关算法和最小绝对收缩与选择算子回归用于特征选择和RS构造。
不同模型的表现对比
DLRN可准确地判定pCR状态,在验证队列中,接收者操作特征曲线下的面积为0.94(95%CI 0.91-0.97),且校准良好。在两个队列中,DLRN表现均优于临床模型和单一RS(p<0.05),还优于两位专家对pCR的预测(p<0.01)。
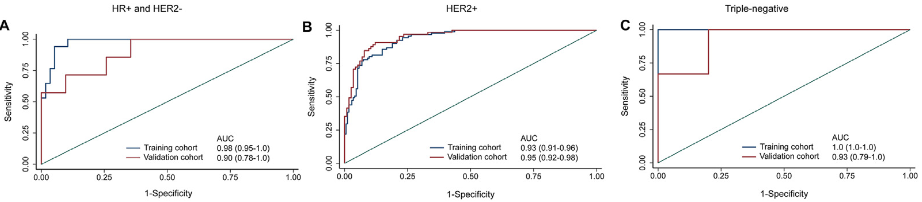
该模型在不同亚型乳腺癌中的表现
此外,该模型在外部验证队列激素受体阳性/人表皮生长因子受体2(HER2)阴性、HER2+和三阴性亚组乳腺癌患者中的也取得了良好的评估识别表现,对应的AUC分别为0.90、0.95和0.93。决策曲线分析证实该模型对临床有用。
综上,这个基因新辅助治疗前后超声影像的深度学习诺模图可准确的评估LABC患者NAC后的pCR情况,为个体化治疗提供信息。
原始出处:
Meng Jiang, et al. Ultrasound-based deep learning radiomics in the assessment of pathological complete response to neoadjuvant chemotherapy in locally advanced breast cancer. Eur J Cancer. February 24, 2021. https://doi.org/10.1016/j.ejca.2021.01.028
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#深度学习模型#
26
#局部晚期#
22
学习了,希望继续努力
70
#完全缓解#
32
#局部#
23
#乳腺癌患者#
25
梅斯里提供了很多疾病的模型计算公式,赞一个!
35