JAMA Netw Open:孕期补充高剂量维生素D并不能改善后代的神经发育
2021-01-24 MedSci原创 MedSci原创
维生素D缺乏症是缺乏维生素D所表现出来的一系列病症,可能是由于摄入的维生素D不足,并且没有接受足够多的阳光照射导致的,也有可能是体内发生的紊乱导致维生素D的吸收受限。
维生素D缺乏症是缺乏维生素D所表现出来的一系列病症,可能是由于摄入的维生素D不足,并且没有接受足够多的阳光照射导致的,也有可能是体内发生的紊乱导致维生素D的吸收受限。维生素D缺乏症是影响各个年龄段和不同种族/族裔人群的主要全球性健康问题。有研究显示,妊娠期维生素D缺乏症与一系列神经发育和精神疾病有关,例如注意力不足/多动症,自闭症和精神分裂症等。然而,关于孕期摄入维生素D水平与新生儿神经发育的关系研究结果尚不一致。
近日,发表在JAMA Netw Open杂志的一项研究显示,与标准推荐剂量(400 IU / d)的维生素D相比,孕期补充高剂量维生素D(2800 IU / d)并不能改善后代神经发育的结果。
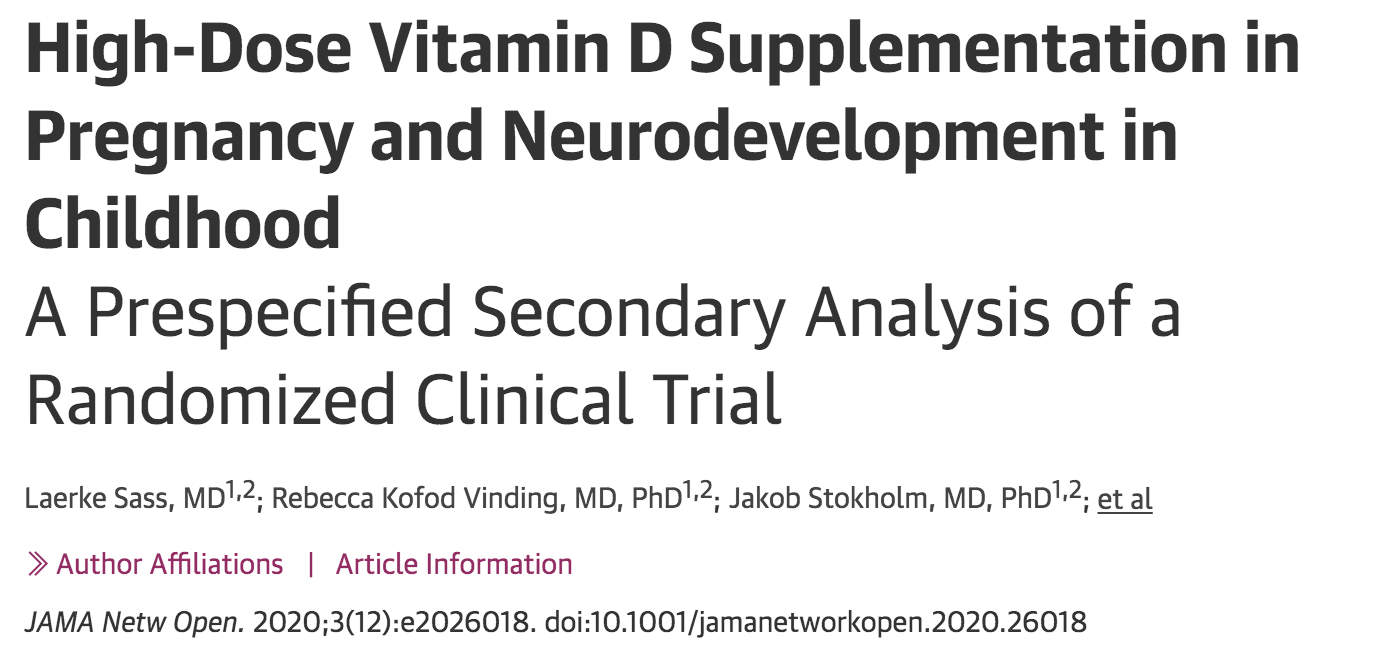
在这项研究中,研究人员对参与2009年3月4日至2010年11月17日COPSAC-2010队列的丹麦623名孕妇进行的双剂量研究:高剂量维生素D组(n=315)和标准剂量组(n=308)。同时,对这些孕妇的孩子进行随访,研究人员对从出生到6岁的551名儿童进行12次随访,其中,高剂量维生素D组(n=277)和标准剂量组(n=274),从而对神经发育进行深度评估。
研究结果显示,在进行语言测试时,孕期补充高剂量维生素D,1岁时词汇量没有改变,而在2岁时的单词量减少,在女孩和男孩中表现出相似的结果。补充高剂量维生素D与标准剂量组相比,认知综合评分没有差异。
另外,在进行神经发育评估时,与标准剂量相比,补充高剂量维生素D对3岁儿童认知综合评分没有影响。然而,女孩的总体运动技能下降,而男孩没有差异。而且,在情绪和行为问卷评分中,不受维生素D摄入水平的影响。
综上所述,与标准推荐剂量的维生素D相比,孕妇在妊娠后期补充高剂量维生素D并不能改善其后代的神经发育。
原始出处
Laerke Sass, High-Dose Vitamin D Supplementation in Pregnancy and Neurodevelopment in Childhood.A Prespecified Secondary Analysis of a Randomized Clinical Trial.JAMA Netw Open. 2020;3(12):e2026018. doi:10.1001/jamanetworkopen.2020.26018
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#高剂量#
39
#PE#
33
#NET#
32
#神经发育#
46
#发育#
40
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
53