JAHA:体重指数对接受室间隔肌切除术肥厚型心肌病患者术后房颤的影响
2022-01-21 MedSci原创 MedSci原创
超重和肥胖是阻塞性肥厚型心肌病患者术后房颤较强的预测因素,通过降低BMI的策略可能是预防术后房颤的潜在手段。
肥厚性心肌病是一种以无法解释病因的左心室肥大为特征的疾病,但没有其他心脏或全身疾病。大约三分之二的肥厚性心肌病患者在静息或激发时表现出左心室流出道梗阻。肥胖是肥厚型心肌病患者已知的心血管危险因素。术后房颤是阻塞性肥厚型心肌病患者术后最常见的并发症之一。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员旨在明确体重指数(BMI)对接受间隔肌切除术的阻塞性肥厚型心肌病患者发生术后房颤的影响。
该研究总共确定了712名既往无房颤且接受了室间隔肌切除术的阻塞性肥厚型心肌病患者。根据BMI将患者分为3组。其中,224人(31.5%)体重正常(BMI<24kg/m2),339人(47.6%)超重(BMI为24至<28kg/m2),149人(20.9%)肥胖(BMI≥28kg/m2)。
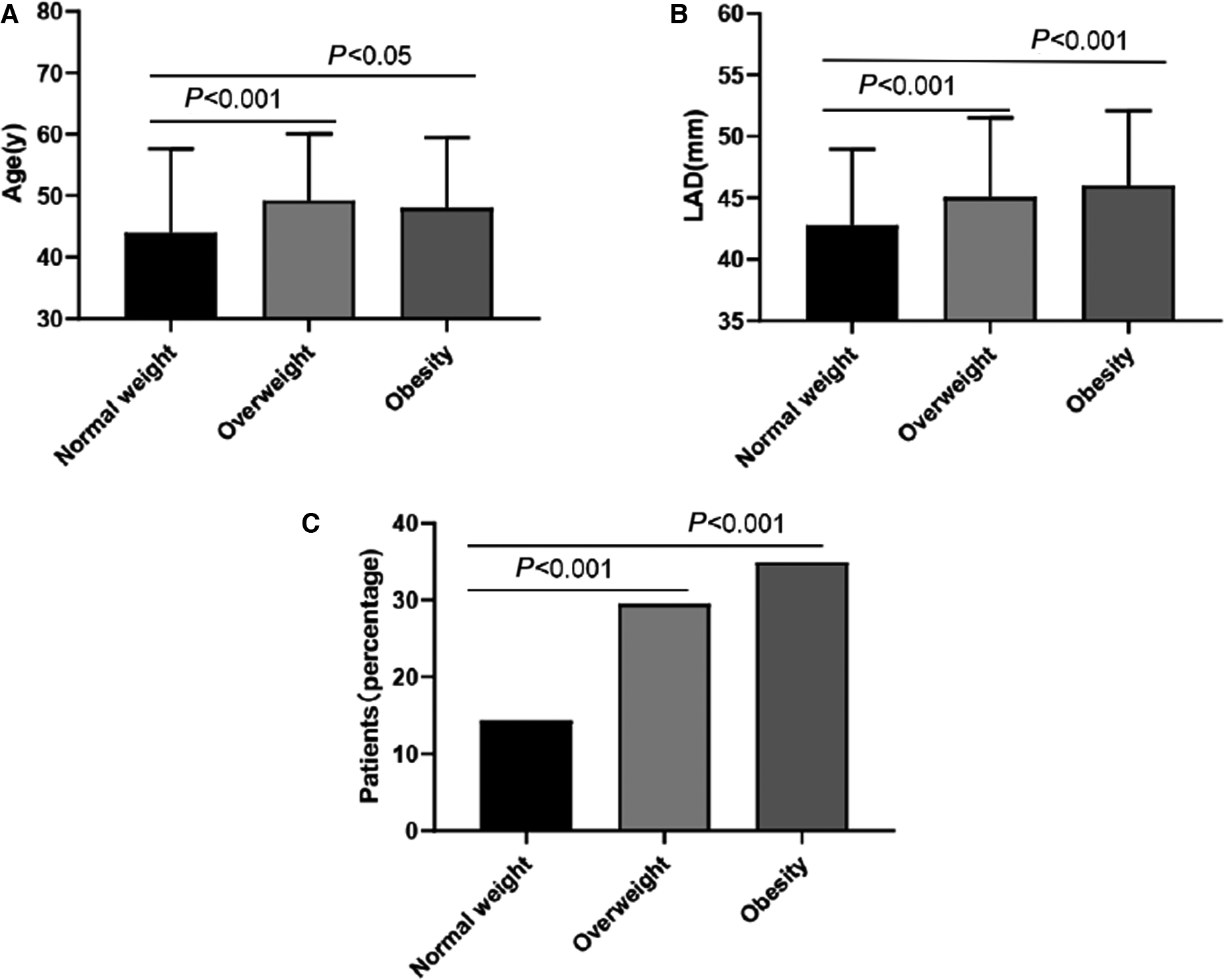
与体重正常的患者相比,超重和肥胖患者的左心房直径(P<0.001)和左心室舒张末期直径(P<0.001)水平增加。在184例(25.8%)发生术后房颤的患者中,正常体重组32例(14.3%),超重组100例(29.5%),肥胖组52例(34.9%)(P<0.001)。Logistic回归分析表明,超重(比值比[OR]为2.161,95%CI为1.333-3.503;P=0.002)或肥胖(OR为2.803;95%CI为1.589-4.944;P<0.001)、年龄(OR为1.037;95%CI为1.018-1.057;P<0.001)和左心房直径(OR为1.060;95%CI为1.027-1.095;P<0.001)与阻塞性肥厚型心肌病患者的术后房颤发生独立相关。
由此可见,超重和肥胖是阻塞性肥厚型心肌病患者术后房颤较强的预测因素,通过降低BMI的策略可能是预防术后房颤的潜在手段。
原始出处:
Jian Zhang.et al.Impact of Body Mass Index on Postoperative Atrial Fibrillation in Patients With Hypertrophic Cardiomyopathy Undergoing Septal Myectomy.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.121.023152
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#室间隔#
41
#术后房颤#
43
#AHA#
40
#肌病#
0
#切除术#
35