激素避孕是预防怀孕的有效方法,几乎适用于所有人。但是,有些人的健康状况可能会增加使用激素避孕药的不良事件风险。此外,有些人同时服用的药物可能会受到激素避孕药的影响或降低其疗效。
既往研究报告指出,普通人群中禁忌采用联合激素避孕的概率在2%~16%之间,但该概率在得克萨斯州育龄的拉丁裔女性研究中更高(39%)。
本研究旨在了解产后女性禁忌采用激素避孕的概率。
研究人员从德克萨斯州的8家医院招募了计划产后推迟2年或更长时间再次生育的低收入产后妇女进行前瞻性队列研究。根据美国疾病控制和预防中心2016年避孕医疗资格标准,女性自我报告的健康状况与激素联合方法和仅使用黄体酮避孕的第3/4类禁忌症相对应。采用混合效应Poisson回归模型来评估与产后6个月内报告的任何禁忌症相关的特征。
有激素避孕禁忌症的概率
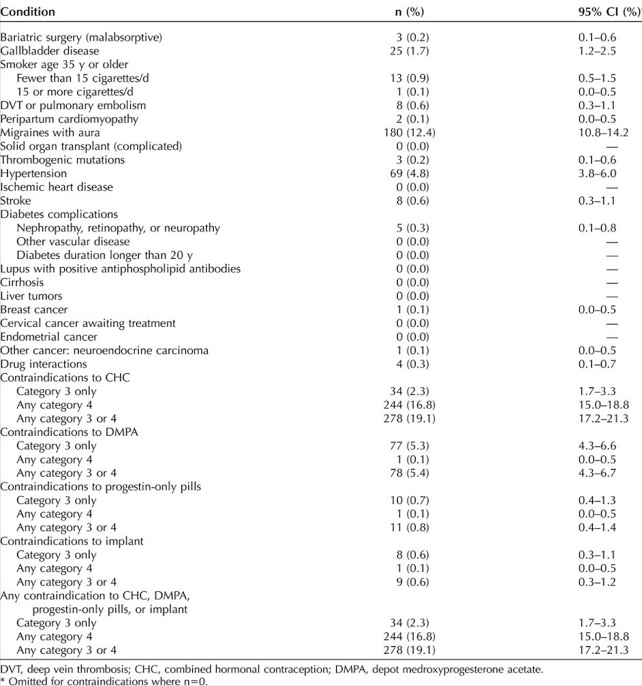
在完成了6个月访谈的1452名女性中,19.1%的人报告了联合激素避孕的第3/4类禁忌症(16.8%的是4类),5.4%的人报告了甲羟孕酮的禁忌症(0.1%的是4类)。只有0.8%的人对只服用黄体酮药片有3/4类禁忌症,0.6%的人对黄体酮植入物有禁忌症。
最常见的禁忌症有先兆偏头痛(12.4%)和高血压(4.8%)。年龄在30岁以上(发生率1.45,95%CI 1.21~1.73)、超重(1.39,1.07~1.80)、肥胖(1.55,1.16~2.07)、有医保(1.34,1.04~1.74)的女性的禁忌采用激素避孕的概率较高。与在美国出生的拉丁裔女性相比,黑人女性有激素避孕禁忌症的概率较高(概率 1.37,95%CI 1.14~1.64),而在外国出生的拉丁裔女性有激素避孕禁忌症的概率较低(0.71,95%CI 0.59~0.86)。
在有禁忌症的女性中,28名(10.3%)使用了联合激素避孕,6名(8%)使用了禁忌达到孕酮方法。
综上,近五分之一的受试者存在3/4类联合激素避孕的禁忌症。不良分娩结局风险较高的患者更有可能有采用激素避孕的禁忌症。
原始出处:
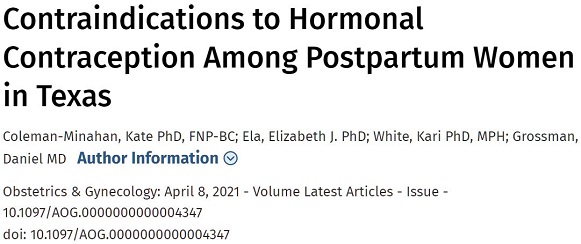
Coleman-Minahan Kate,Ela Elizabeth J,White Kari et al. Contraindications to Hormonal Contraception Among Postpartum Women in Texas. Obstet Gynecol, 2021, https://doi.org/10.1097/AOG.0000000000004347
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#NEC#
36
#TET#
48
比较担心致癌的副作用,没有提及
56
学习学习
62
#禁忌#
0
看
69