J Periodontol:睡眠与重度牙周炎之间相关性的研究
2020-06-27 MedSci原创 MedSci原创
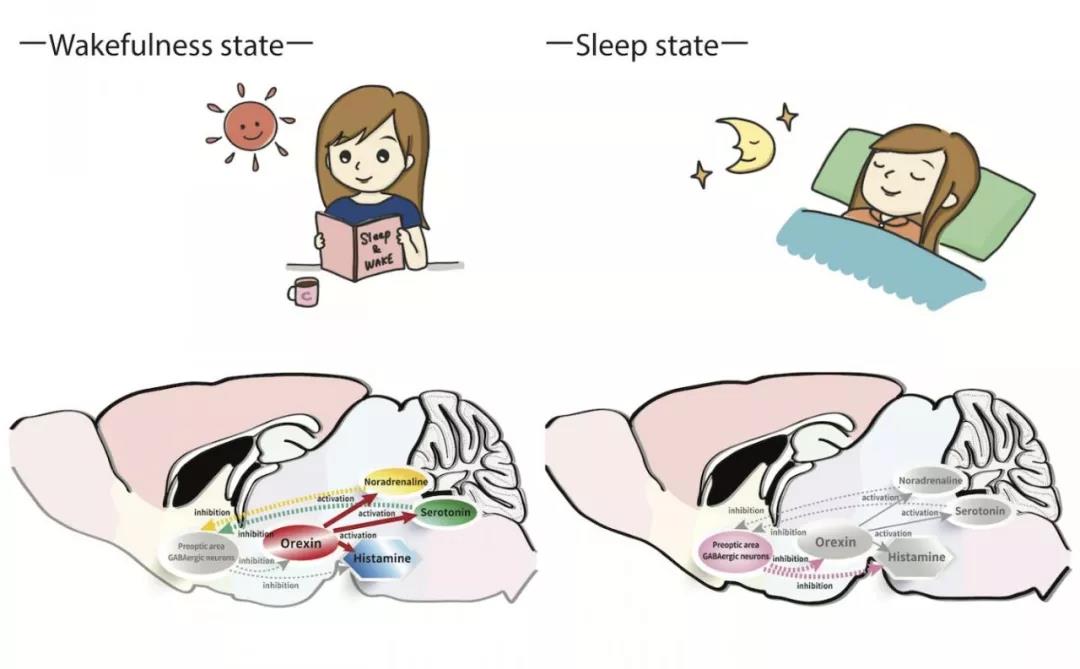
不良的睡眠行为似乎会通过代谢失调和免疫抑制而对健康产生不利影响。睡眠障碍与糖尿病,心血管疾病和某些癌症密切相关。
不良的睡眠行为似乎会通过代谢失调和免疫抑制而对健康产生不利影响。睡眠障碍与糖尿病,心血管疾病和某些癌症密切相关。本研究旨在评估美国国家人口健康与营养调查(NHANES)中一项美国人口研究中的睡眠时间与牙周疾病之间的关联。
研究收集年龄≥30岁的个体,包括美国NHANES 2013-2014年的3,624名参与者。加权多变量logistic回归模型量化了睡眠与重度牙周疾病之间的相关性。检测糖尿病是否可以作为效应修饰因子,并针对潜在的混杂因素进行了调整,例如吸烟状况,性别,年龄,教育程度和就诊时间。
结果发现,根据年龄,性别,吸烟状况,FPL,教育程度和牙科就诊次数进行调整后,睡眠时间> 7h/night且无睡眠困难的个体患重度牙周疾病的可能性降低40%(odds ratio[OR] = 0.6,P <0.05)。此外,糖尿病是睡眠与重度牙周病相关性的重要修饰因子(OR = 4.8,P <0.05)。
因此,睡眠时间与重度牙周炎之间的相关性具有统计学意义。睡眠时间> 7h/night的出现重度牙周疾病的可能性降低。与没有糖尿病的人相比,这种关系在患有糖尿病的人群中更明显。
原文出处:
Hend Alqaderi,Association between sleep and severe periodontitis in a nationally representative adult US population. Journal of periodontology, 2020 June. Doi: 10.1002/JPER.19-0105
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
28
#重度牙周炎#
38
#相关性#
30
好用
0
好用
109
#牙周#
25