Ann Intern Med:心衰患者钠-葡萄糖共转运蛋白2抑制剂的效果分析
2022-04-16 MedSci原创 MedSci原创
随机对照试验确定了钠-葡萄糖协同转运蛋白2(SGLT2)抑制剂对2型糖尿病患者具有心脏保护作用。新的证据表明,这些结果可以扩展到没有糖尿病的个体。
随机对照试验确定了钠-葡萄糖协同转运蛋白2(SGLT2)抑制剂对2型糖尿病患者具有心脏保护作用。新的证据表明,这些结果可以扩展到没有糖尿病的个体。

近日,内科学权威杂志Annals of Internal Medicine上发表了一篇研究文章,该研究旨在评估SGLT2抑制剂对心力衰竭患者的影响,无论是否伴有2型糖尿病。
研究人员检索了PubMed、Web of Science、Cochrane图书馆和Embase(OVID界面)。符合条件的试验将患有心力衰竭的成人随机分配到SGLT2抑制剂组或对照组。研究人员从已发表的Kaplan-Meier图重建事件发生时间的个体患者数据,并使用简单模型计算了半年、1年和2年的时间范围内计算时变风险比(RR)。
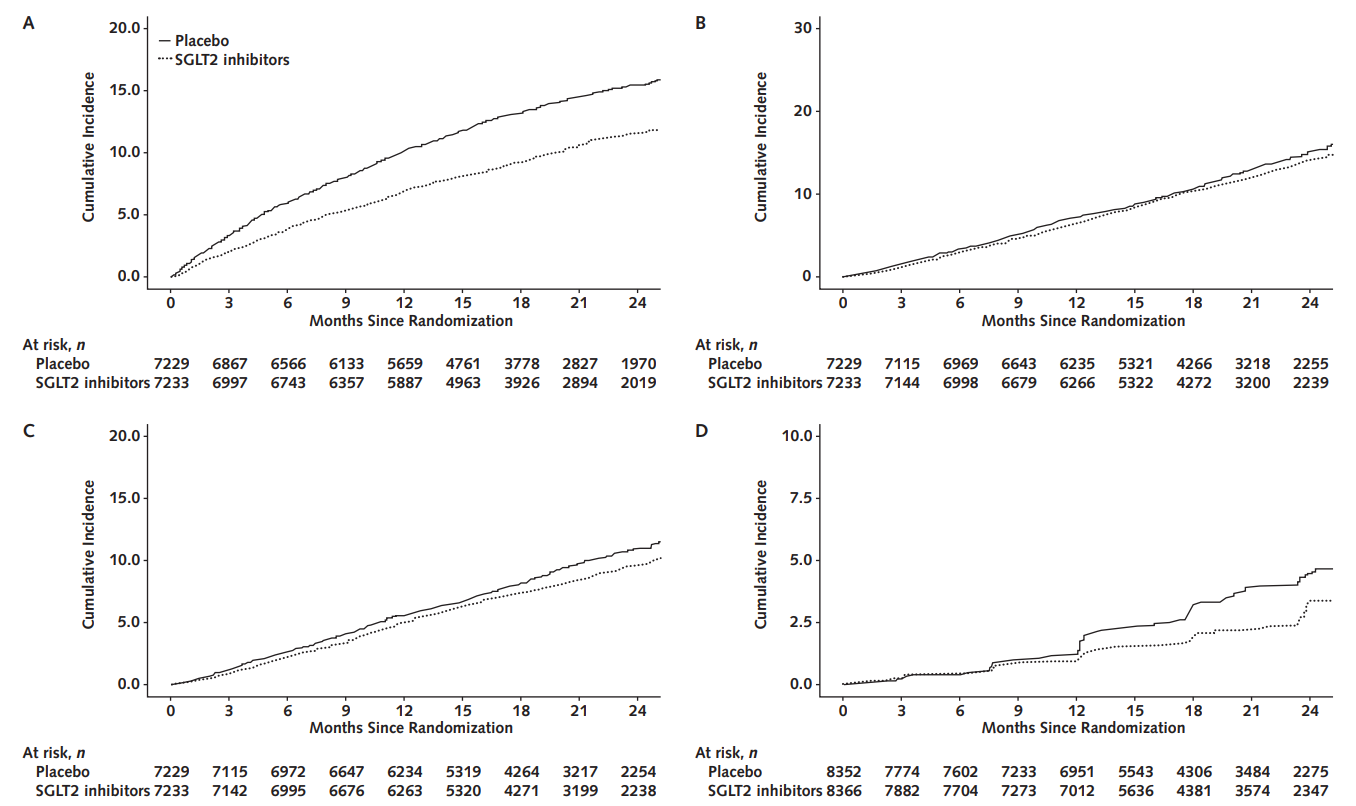
钠-葡萄糖协同转运蛋白2抑制剂在6个月时将心力衰竭住院率降低37%(95%CI为25%至47%),在1年时降低32%(95%CI为20%至42%),在2年时26%(95%CI为10%至40%),并在1年将心血管死亡减少14%(95%CI为1%至25%)(高确定性)。然而,低质量证据并未表明可以预防全因死亡、肾病进展或肾衰竭。对于在第一年接受治疗的患者和预后较差的患者(例如在医院新诊断为心力衰竭的患者),预期的绝对收益更大。此外,SGLT2抑制剂使生殖器感染的风险加倍(RR为2.69[CI为1.61至4.52];高确定性)。
由此可见,在心力衰竭患者中,SGLT2抑制剂可减少心力衰竭住院率,无论是否伴有糖尿病;绝对获益在治疗第一年中最为显著,并因预后因素而异。临床医生应注意接受SGLT2抑制剂的患者生殖器感染风险增加。
原始出处:
Xinyu Zou,et al. Sodium–Glucose Cotransporter-2 Inhibitors in Patients With Heart
Failure A Systematic Review and Meta-analysis.Ann Intern Med 2022.https://www.acpjournals.org/doi/pdf/10.7326/M21-4284
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#转运#
39
#效果分析#
36
#抑制剂#
41
#2抑制剂#
42
#心衰患者#
48
#Med#
33