Eur Urol:前列腺手术后男性尿道压力性尿失禁手术的非劣效性随机对照试验结果(MASTER)
2021-02-21 AlexYang MedSci原创
压力性尿失禁(SUI)是前列腺根治性切除术后的常见病,尽管进行了保守治疗,但很可能持续存在。吊带是一种新兴的治疗持续性SUI的手术,但缺乏与既有的人工尿道括约肌(AUS)的随机对照试验(RCT)比较。
压力性尿失禁(SUI)是前列腺根治性切除术后的常见病,尽管进行了保守治疗,但很可能持续存在。吊带是一种新兴的治疗持续性SUI的手术,但缺乏与既有的人工尿道括约肌(AUS)的随机对照试验(RCT)比较。
最近,有研究人员比较了前列腺手术后尿流动力学SUI困扰的男性的手术效果。研究共包括了380名参与者。在随机化后第12个月,男性吊带的尿失禁率为134/154(87.0%),而AUS的尿失禁率为133/158(84.2%)(差异3.6%[95%CI-11.6至4.6],pNI=0.003),显示出非劣效性。失禁症状(ICIQ-UI SF)从基线时的16.1分和16.4分分别降低到8.7分(吊带)和7.5分(AUS)(平均差异1.4[95%CI 0.2到2.6],p=0.02)。严重的AEs(SAE)很少:吊带和AUS分别有6名和13名(一名男性有3个SAE)。生活质量评分有所改善,两组的满意度都很高。所有其他次要结果表明AUS更优。
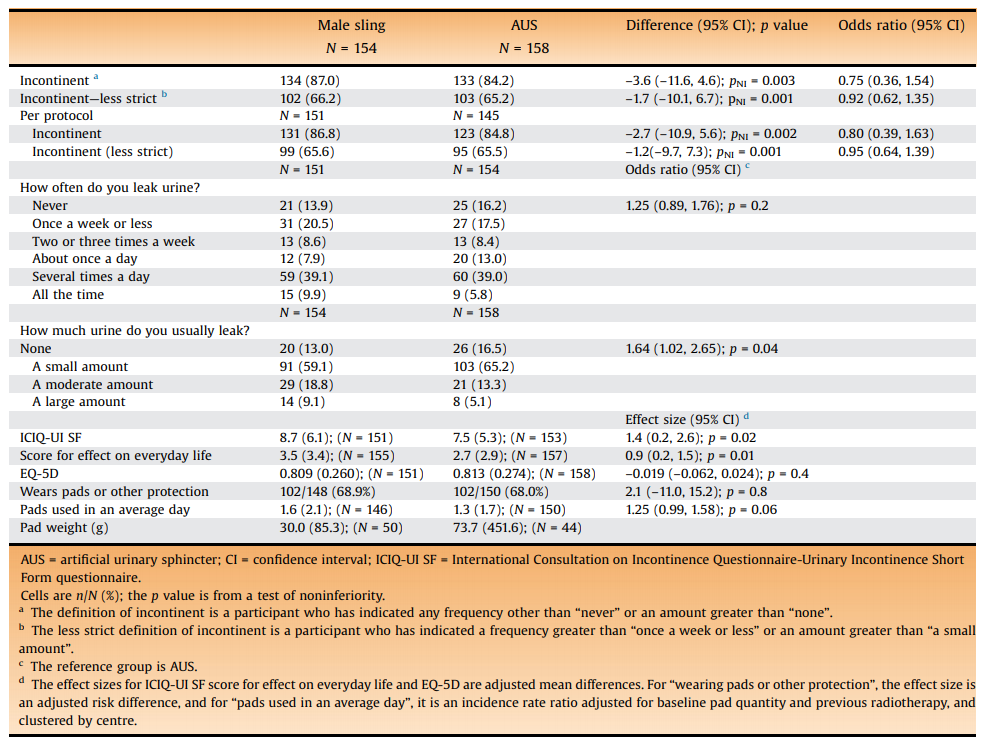
最后,研究人员指出,尿失禁率较高且没有证据表明男性吊带和AUS之间存在差异。两组的症状和生活质量均有明显改善,男性对两种手术普遍满意。总的来说,二次分析和事后分析都有利于AUS。
原始出处:
Paul Abrams , Lynda D Constable , David Cooper et al. Outcomes of a Noninferiority Randomised Controlled Trial of Surgery for Men with Urodynamic Stress Incontinence After Prostate Surgery (MASTER). Eur Urol. Feb 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#AST#
41
#非劣效性#
40
#对照#
38
#对照试验#
45
#尿道#
44
#非劣效#
29
#尿失禁#
51
#随机对照试验#
37
高质量研究,读起来真爽,谢谢梅斯
54
好文章!
103