中国研究人员21日在新一期美国《科学—转化医学》杂志上报告说,一种结合使用抑制剂与化疗药物的联合用药方案也许能有效对抗肾癌的耐药性,提高治疗效果。科学家说,这是逆转肾癌耐药研究方面取得的重要进展。
肾癌,全称肾细胞癌,发病率在中国泌尿生殖系统肿瘤中位居第二位。早、中期肾癌首选手术治疗,但晚期转移性肾癌对大部分化疗药物耐药,一直没有好的治疗办法。
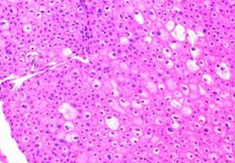
中国浙江大学药学院的曾苏和余露山等人从提高药物转运蛋白活性、增加癌细胞中化疗药物浓度进而逆转耐药、提高疗效的思路出发,通过对大量临床样本的筛选分析,发现肾癌患者中一种负责将药物转运至癌细胞的转运蛋白的表达显著下降。
进一步研究发现,DNA(脱氧核糖核酸)甲基化对肾癌中这种名为OCT2蛋白表达的下降发挥了重要作用。为此,研究人员设计了DNA甲基转移酶抑制剂地西他滨与抗癌药物奥沙利铂的联合用药方案。
动物实验中,接受治疗的小鼠肾癌组织中OCT2蛋白的表达水平明显升高,奥沙利铂在肾癌组织中积聚,取得显著的抗癌作用。
研究人员说,这项成果不仅对肾细胞癌的治疗具有积极的意义,也为其他先天耐药性肿瘤的治疗提供了思路。《科学转化医学》杂志的编辑认为,这项研究“打开了进入癌细胞的一扇门”。
原始出处
Yanqing Liu1,*, Xiaoli Zheng1,*, Qinqin Yu1, Hua Wang2, Fuqing Tan3, Qianying Zhu1, Lingmin Yuan1, Huidi Jiang1, Lushan Yu1,†,‡ and Su Zeng1,†.Epigenetic activation of the drug transporter OCT2 sensitizes renal cell carcinoma to oxaliplatin.Science Translational Medicine.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#中国科学#
34
#TRA#
30
好好学习
69
#中国科学家#
39
#Med#
31