Circulation:房颤持续时间和CHA2DS2-VASc评分对卒中风险的预测意义
2019-11-16 QQY MedSci原创
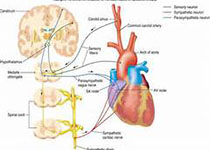
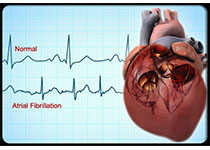
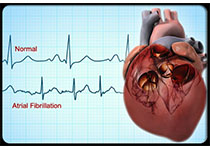
心血管植入电子设备患者的相关研究表明房颤(AF)持续时间与卒中风险之间具有相关性,但与CHA2DS2-VASc评分之间的关系尚无明确数据。现Kaplan等人根据CHA2DS2-VASc评分和AF持续时间来评估心血管植入电子设备患者的卒中和系统栓塞率(SSE)。研究人员将Optum电子健康记录鉴定数据库(2007-2017)的数据与Medtronic CareLink心血管植入电子设备数据库链接起来
现Kaplan等人根据CHA2DS2-VASc评分和AF持续时间来评估心血管植入电子设备患者的卒中和系统栓塞率(SSE)。研究人员将Optum电子健康记录鉴定数据库(2007-2017)的数据与Medtronic CareLink心血管植入电子设备数据库链接起来,该数据库能够持续监测AF。筛选设备植入6个月或电子健康记录数据可用1年后的数据。
共纳入21 768位心血管植入电子设备的非抗凝患者(68.6±12.7岁,63%为男性),AF持续时间延长和CHA2DS2-VASc评分增加均与SSE年化风险显著相关(P<0.001)。在无论AF持续时间长短,CHA2DS2-VASc评分0-1分时,SSE发生率较低。但CHA2DS2-VASc评分为2分、房颤持续时间>23.5h的患者,CHA2DS2-VASc评分3-4分、房颤持续时间>6min的患者和CHA2DS2-VASc评分≥分(无论有无房颤)的患者,卒中风险均超过可控的阈值,即>1%/年。
综上所述,AF持续时间与CHA2DS2-VASc评分之间存在交互作用,可以进一步将AF患者进行SSE风险分层,或可助于指导抗凝治疗。
原始出处:
Rachel M. Kaplan, et al.Stroke Risk as a Function of Atrial Fibrillation Duration and CHA2DS2-VASc Score.Circulation. 2019;140:1639–1646
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CHA2#
45
#ASC#
43
#CHA2DS2-VASc评分#
0
#卒中风险#
38
#持续时间#
44
#CHA2DS2-VASc#
39
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
49
房颤,临床上碰到很多哦
0
中风是俗称,应该称为缺血性卒中吧
43
非常受益,很好的研究
86