Arterioscler Thromb Vasc Biol:抑制CHK 1(检查点激酶1)可以治疗肺动脉高压
2020-04-20 MedSci原创 MedSci原创
肺动脉高压(PAH)是一种衰弱性疾病,与肺动脉远端血管重塑有关,导致肺动脉压力升高、右心室肥大和死亡。虽然呈现出高水平的DNA损伤,通常会危及其生存能力,但肺动脉平滑肌细胞(PASMCs)从PAH患者
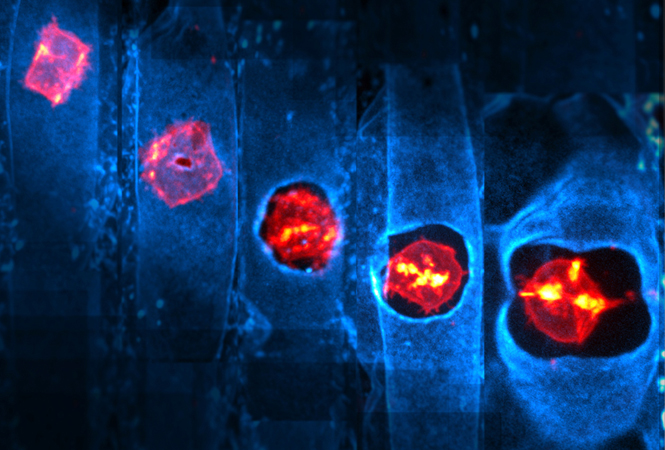
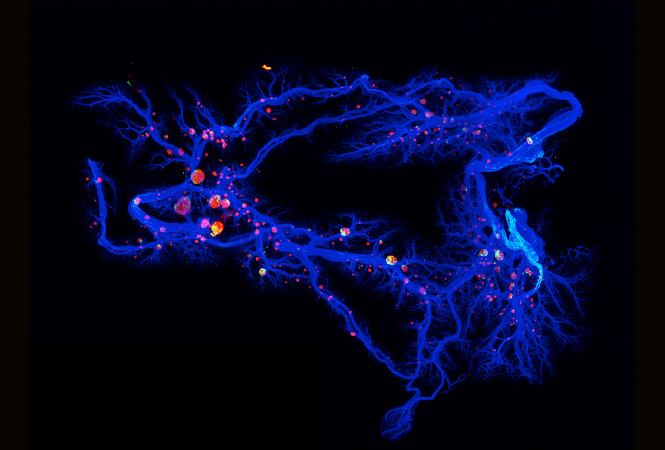
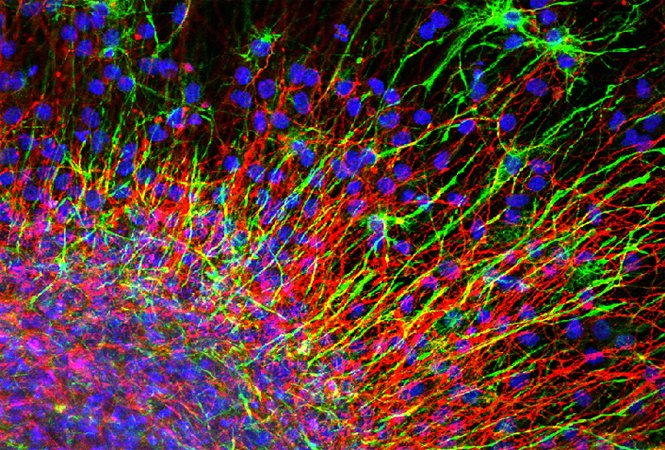
肺动脉高压(PAH)是一种衰弱性疾病,与肺动脉远端血管重塑有关,导致肺动脉压力升高、右心室肥大和死亡。虽然呈现出高水平的DNA损伤,通常会危及其生存能力,但肺动脉平滑肌细胞(PASMCs)从PAH患者的肺动脉平滑肌细胞(PASMCs)表现出类似癌症的增殖和抗凋亡表型,是导致血管腔湮灭的原因。在癌细胞中,丝氨酸/苏氨酸蛋白激酶CHK1(checkpoint kinase 1)的过量表达被利用来抵消它们所受到的过量的DNA损伤侵袭。本研究旨在确定PAH-PASMCs是否形成了由CHK1介导的协调反应,以克服DNA损伤,使细胞存活和增殖。
结果显示,与对照组相比,CHK1的表达在分离的PASMCs和PAH患者的远端PAs中明显增加,并且在多个辅助动物模型中重述了该疾病,包括单核细胞移植大鼠和猿猴免疫缺陷病毒感染的猕猴。使用药理和分子功能丧失方法,我们发现CHK1促进PAH-PASMCs增殖和抗凋亡。此外,我们发现抑制CHK1会诱导DNA修复蛋白RAD 51的下调和严重的DNA损伤。在体内,我们发现,药理抑制CHK1显著减少血管重塑,改善了2个实验性大鼠模型的PAH的血流动力学参数。
综上所述,该研究结果表明,CHK1通过减轻DNA损伤在PAH-PASMC中发挥促增殖作用,提示CHK1抑制可能是PAH患者有吸引力的治疗选择。
原始出处:
Alice Bourgeois, Sébastien Bonnet, et al., Inhibition of CHK 1 (Checkpoint Kinase 1) Elicits Therapeutic Effects in Pulmonary Arterial Hypertension. Arterioscler Thromb Vasc Biol. 2019 Aug; 39(8): 1667–1681. doi: 10.1161/ATVBAHA.119.312537
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#肺动脉高压#
138
#动脉高压#
28
#Biol#
34
#ASC#
25
#Bio#
37
#ART#
30
#激酶#
31
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
49