JACC:改良的非缺血扩张型心肌病患者室性心律失常和猝死风险分层
2021-06-20 Nebula MedSci原创
改良的非缺血扩张型心肌病患者室性心律失常和猝死风险分层
非缺血性扩张型心肌病(DCM)患者发生室性心律失常(VA)和猝死的传统风险分层是基于左心室射血分数(LVEF)。但是,单纯LVEF并不是心律失常终点的一个非常准确的预测指标,因此,室性心律失常(VA)和猝死的传统风险分层方法仍有待优化。
本研究旨在提供一种改进的对DCM患者进行VA和猝死风险分层的算法。
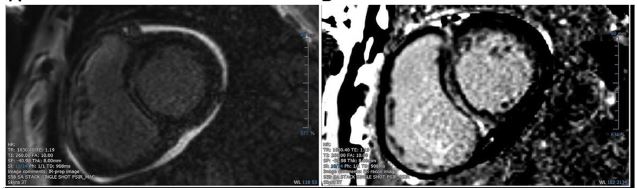
晚期钆增强(LGE)心脏磁共振检查
这是一项回顾性的队列研究,纳入了在2个三级转诊中心接受晚期钆增强(LGE)心脏磁共振检查的连续DCM患者。联合心律失常终点包括植入式心律转复除颤器治疗、持续性室性心动过速、心脏骤停复苏和猝死。
结合了LGE和LVEF的预测模型
共纳入了1165位患者,中位随访了36个月,LGE是心律失常终点独立的强有力的预测指标(风险比 9.7;p<0.001)。这种相关性在左心室射血分数(LVEF)不同的患者中都是一致的。心外膜LGE、跨壁LGE、合并室间隔和游离壁LGE均与高心律失常风险相关。
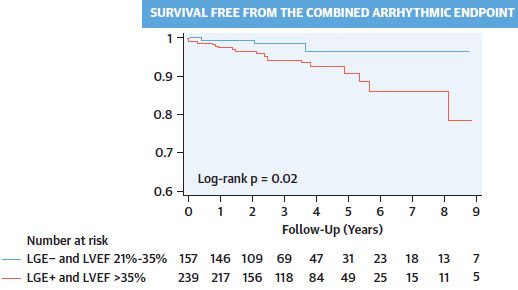
LVEF 21-35%的LGE阴性患者和LVEF>35%的LGE+患者的心律失常终点
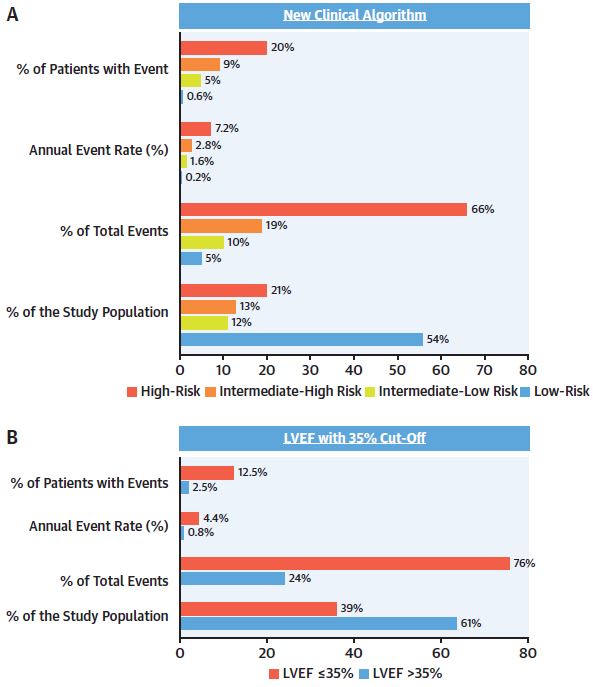
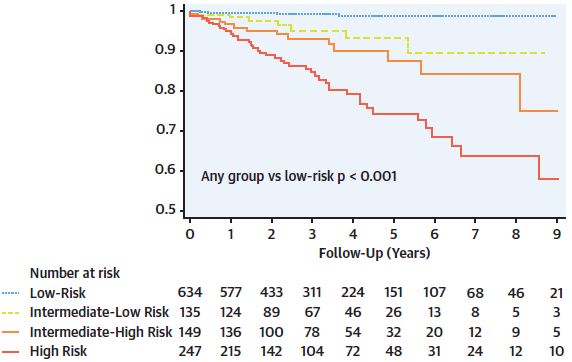
结合LGE和3个LVEF分层(即≤20%、21%-35%、>35%)的简单算法明显优于LVEF 35%阈值(Harrell's C统计值:0.8 vs 0.69;曲线下面积:0.82 vs. 0.7;p<0.001),可对34%的DCM患者的心律失常风险进行重新分类。LVEF 21%-35%的LGE阴性患者的心律失常风险较低(年发生率 0.7%),而高LGE分布风险的LVEF>35%的患者的心律失常风险较高(年发生率 3%;p=0.007)。
新算法不同风险分层患者无联合心律失常终点生存期
总而言之,该DCM患者队列显示,LGE是VA或猝死的一个显著的、一致的、强有力的预测指标。心外膜LGE、跨壁LGE、合并室间隔和游离壁LGE是特异性的高风险LGE分布。整合了LGE和LVEF的临床算法可显著提高与植入式转复除颤器相关的VA和猝死风险分层。
原始出处:
Di Marco Andrea,Brown Pamela Frances,Bradley Joshua et al. Improved Risk Stratification for Ventricular Arrhythmias and Sudden Death in Patients With Nonischemic Dilated Cardiomyopathy.[J] .J Am Coll Cardiol, 2021, 77: 2890-2905. https://doi.org/10.1016/j.jacc.2021.04.030
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
29
#扩张#
30
#ACC#
38
#风险分层#
38
#猝死风险#
47
#肌病#
34