EBioMedicine:预测1型糖尿病微血管并发症5年风险的精确诊断方法
2022-05-21 从医路漫漫 MedSci原创
高血糖是1型糖尿病这两种并发症发病的最重要的已知预测因子。肾小球滤过率(GFR)和尿白蛋白排泄率本身也是糖尿病肾病进一步进展的主要预测因子。
背景:糖尿病的破坏性微血管并发症(DC),如糖尿病肾病(DN)和糖尿病视网膜病变(DR),导致糖尿病患者死亡率、失明、肾功能衰竭和总体生活质量下降。全身性高血糖水平导致视网膜毛细血管内皮细胞和肾小球系膜细胞的损伤。因此,高血糖是1型糖尿病这两种并发症发病的最重要的已知预测因子。肾小球滤过率(GFR)和尿白蛋白排泄率本身也是糖尿病肾病进一步进展的主要预测因子。虽然临床危险因素和血糖控制可以很好地预测微血管并发症的发展,但在疾病的早期阶段,它们不一定准确。因此,需要一种能够利用隐藏的风险模式和分子动力学,从而实现对DC的准确预测。
代谢组学和脂类组学是新陈代谢的快照,可以应用于糖尿病的研究,以获得全面的分子图谱。在过去的十年中,组学技术已经显示出以一种以前无法想象的方式对患者进行个性化护理的潜力。因此,通过将已知的临床风险因素与广泛的组学小组相结合,我们的目标是研究进展为DR和糖尿病肾病过程中的生物动力学。机器学习(ML)算法从大量数据中学习描述性模式。因此,这项技术的应用可以支持临床决策,也是近年来人工智能影响最大的领域之一。ML可以增强医疗保健专业人员的能力,到目前为止,它已有效地应用于预测糖尿病患者的心力衰竭和视网膜病变的风险。使用ML算法预测其他情况正在取得重大进展。在糖尿病肾病(DKD)的情况下,已经进行了广泛的研究,以寻找未来终末期肾脏疾病的预测生物标志物。然而,据作者所知,没有一项研究使用ML来预测1型糖尿病估计肾小球滤过率(EGFR)下降的进展。另一方面,在DR并发症的情况下,最近报道和提交了数百项具有高度预测性方法的出版物和专利,包括基于深度学习的视网膜图像分析。
目的:在哥本哈根Steno糖尿病中心(SDCC)的一个大型且特征良好的1型糖尿病队列中,我们试图为DC开发易于解释和准确的预后风险预测模型。为此,我们将ML与临床数据相结合,结合两组组学数据来预测随访数据中的DC进展。在这项研究中,我们假设1 ML可以用于使用标准的临床危险因素预测1型糖尿病未来的并发症;2结合基于血液的代谢表型和临床数据将通过模拟危险因素和分子代谢之间的动力学来改进预测。本研究的最终目的是为DC设计一种可应用于临床的个性化风险预测工具。
方法:利用537名成人1型糖尿病(T1D)患者队列中的数据,我们预测了5年内进展为DCs的情况。预测模型首先用基线的临床危险因素进行计算,然后用基线的临床危险因素和血源性分子数据进行计算。在两个并发症特异性模型中预测了糖尿病肾病和糖尿病视网膜病变的进展。
研究结果:该模型预测糖尿病肾病进展的准确度为:0.96±0.25和0.96±0.06曲线下面积,AUC,分别采用临床测量和小分子预测因子,并强调主要预测因子为蛋白尿、肾小球滤过率、基线视网膜病变状态、糖衍生物和酮。对于糖尿病性视网膜病变,AUC分别为0.75±0.14和0.79±0.16,具有临床测量值和小分子预测值,并突出了关键预测值、蛋白尿、肾小球滤过率和基线视网膜病变状态。建立个体风险评分以可视化结果。
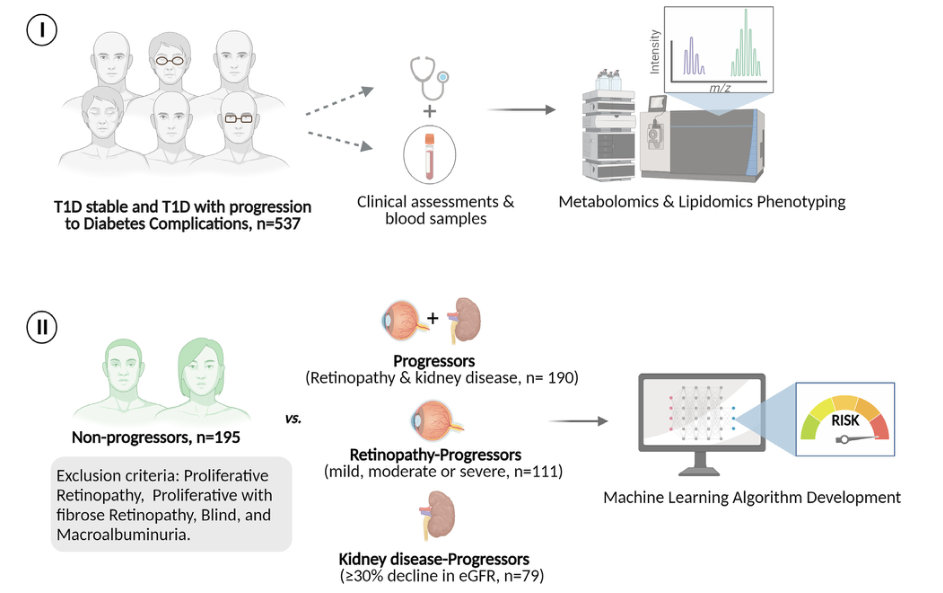
图1.研究设计和机器学习含义的图形表示。从537名1型糖尿病患者(I)中收集了基线临床数据和血浆样本(代谢组学和血脂组学分析)。参与者被分成两组:1型糖尿病稳定组(n=195)或1型糖尿病伴糖尿病并发症进展组(n=190)。合并糖尿病并发症、糖尿病肾病(EGFR下降30%;n=79)和糖尿病视网膜病变(轻、中、重度;n=111)的进展被预测(Ii)。中位随访期为5.4年。
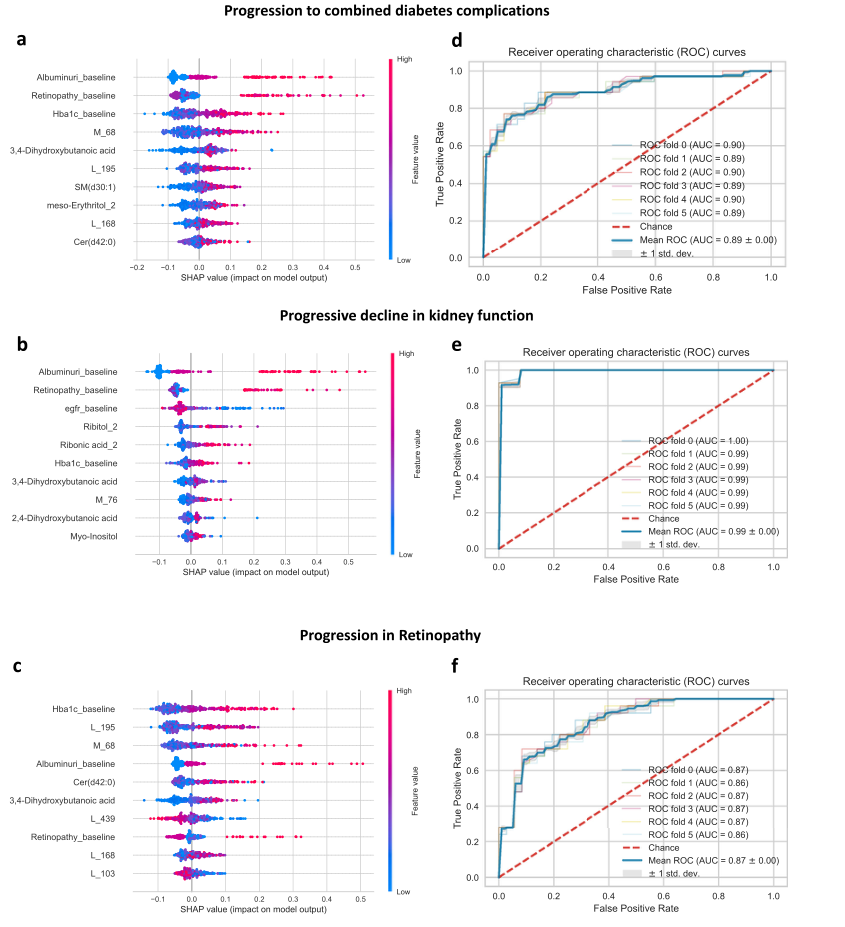
图2.基于临床和组学特征的模型。(a?c)点图的子集,显示使用临床数据预测代谢物水平(y轴)的五重交叉验证模型计算出的各种特征(x轴)的方向平均绝对Shap值。在验证集中,正Shap值和负Shap值分别对糖尿病合并并发症(A)、EGFR下降30%(B)和视网膜病变(C)的预测进展风险产生积极和消极影响。正(负)Shap值表示较高(较低)的特征值平均导致较高的预测值。每个图由验证数据集中的各个点组成,较高的值为红色,较低的值为蓝色。显示的是所有临床数据的最大平均绝对形状值的最高特征。(d-f)AUROC、Mean和SD由基于主要预测因子的模型得到。MC获得的糖尿病并发症、糖尿病肾病和糖尿病视网膜病变的100个AUROC值的平均值和SD分别为0.84±0.11、0.97±0.05和0.87±0.10(未显示)。特征标签是:视网膜病变_基线(1=无明显,2=轻度非增殖性,3=中度非增殖性);白蛋白尿_基线(1=正常蛋白尿,2=微量蛋白尿,3=大量蛋白尿)。

图3.基于临床特征的随机森林模型的可视化。A,该图显示了使用随机森林计算的树的示例。这是500个计算决策树中的一个例子,用于对临床数据集进行分类,以预测EGFR下降30%。B,500个决策树中的一个的例子,用于分类临床数据集以预测视网膜病变。每一类用一种颜色表示(在a中是棕色和蓝色,在(B)中是紫色和绿色,链接的宽度表示从一个节点流向另一个节点的数字项。
结果:用进一步验证的ML工具进行解释可以促进临床上精确诊断的实施。据设想,可以在并发症发生之前对患者进行筛查,从而保护糖尿病患者的健康寿命。
原文出处:Al-Sari N, Kutuzova S, Suvitaival T, et al.Precision diagnostic approach to predict 5-year risk for microvascular complications in type 1 diabetes.EBioMedicine 2022 May 06;80
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#CIN#
41
#微血管并发症#
54
#Bio#
37
#并发#
57
#诊断方法#
50
#EBI#
36
#DIC#
24
#微血管#
42
#血管并发症#
39
#Medicine#
27