肝细胞癌(HCC)是全球第六大最常见癌症,也是第四大最常见的癌症相关死亡原因。病毒性肝炎是肝癌的常见原因,而我国恰恰是肝炎大国,我国有很高的肝癌负担。虽然现在很多研究都集中在肝癌的致病基因特征,但是,中国HCC患者的遗传图谱尚未有充分研究。
本研究旨在解析中国HCC患者的遗传特征。
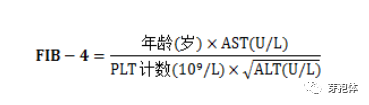
共招募了165位HCC患者,包括146位男性和19位女性。中位年龄为55岁(范围 27-78岁)。同时采集了患者的相应的临床和病理信息。共收集了168份肿瘤组织以进行二代测序(NGS),涵盖450个基因。检测的变异包括单核苷酸变异(SNV)、小片段和长片段插入和缺失(InDels)、拷贝数变异和基因重组。此外,还分析了肿瘤突变负荷(TMB),最高四分位的HCC被划分为高TMB。
突变图谱
在168份HCC组织中的258个基因中共检测出了1004个遗传变异。确定了160份HCC样本的TMB值,中位TMB值为5.4 Muts/Mb(范围 0-28.4 Muts/Mb),75% TMB线为7.7 Muts/Mb。最常见的突变基因有TP53、TERT、CTNNB1、AXIN1、RB1、TSC2、CCND1、ARID1A和FGF19。SNV是最常见的突变类型,G:C>T:A和鸟嘌呤转化是最常见的SNV。
与野生型患者相比,携带TP53突变的患者中Edmondson III-IV级和微血管浸润的比例明显较高(p<0.05)。在TERT突变的患者中,肿瘤侵犯肝包膜的比例明显更高(p<0.05)。在CTNNB1突变患者中,Edmondson I-II级、甲胎蛋白(AFP) <25 μmg/L和无乙肝病史的比例显著升高(p<0.05)。CTNNB1突变与高TMB相关(p<0.05)。
相关分析显示,TP53突变与微血管侵袭(p=0.002, OR=3.096)和Edmondson III-IV级独立相关(p=0.008, OR=2.613)。TERT突变与肝包膜肿瘤浸润独立相关(p=0.001, OR=3.030)。CTNNB1突变与AFP独立相关(<25 μmg/L) (p=0.009, OR=3.414)。
综上所述,中国HCC患者最常见的突变基因有TP53、TERT和CTNNB1,这些基因可能通过调节TP53通路、Wnt信号通路和端粒修复通路导致HCC的发生发展。而且,携带不同基因突变的患者往往有不同的临床特征。
原始出处:
Wang Shuo,Shi Huasheng,Liu Tao et al. Mutation profile and its correlation with clinicopathology in Chinese hepatocellular carcinoma patients. Hepatobiliary Surg Nutr, 2021, 10: 172-179.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#肝癌患者#
47
学习
49
#EPA#
37
#Biliary#
54
赞
65
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
49