Lung Cancer:真实世界研究中评估免疫治疗一线治疗晚期非小细胞肺癌(NSCLC)患者的疗效
2021-07-01 yd2015 MedSci原创
真实世界研究评估的,免疫治疗一线治疗晚期非小细胞肺癌(NSCLC)患者的生存较临床研究的要低,表明对此需要进一步改进治疗措施。
对于EGFR和ALK突变阴性的转移性非小细胞肺癌(NSCLC),目前一线治疗推荐免疫治疗单药或联合化疗。临床研究已经证实一线的免疫治疗可以改善晚期NSCLC患者的预后。如KEYNOTE-042研究证实,PD-L1≥1%患者中,帕博利珠单抗对比化疗的中位OS为16.7个月 vs. 12.1个月;KEYNOTE-407研究中,帕博利珠单抗联合化疗对比单纯化疗的中位OS为17.1 个月vs. 11.6个月;KEYNOTE-189研究中,帕博利珠单抗联合化疗对比单纯化疗的中位OS为22.0个月vs. 10.6个月;IMpower150研究中,阿替利珠单抗联合治疗组对比化疗的中位OS为19.5个月 vs. 14.7个月。但是真实世界中,免疫治疗的疗效以及长期获益不是很明确。因此,美国研究者开展了一项真实世界研究,评估免疫治疗(I-O)一线治疗晚期NSCLC患者的疗效。相关研究发表在Lung Cancer杂志上。
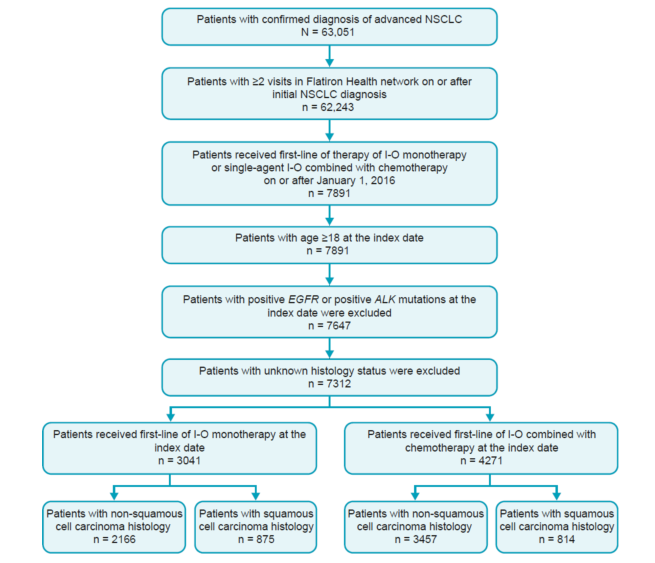
研究纳入标准:年龄≥18岁,分期为III–IV的NSCLC患者,接受一线免疫单药或免疫联合化疗治疗。研究评估总生存(OS)和无进展生存(PFS)。63,051例患者诊断为晚期NSCLC,其中4271例患者接受I-O联合化疗,3041例患者接受单药I-O。
研究概况
4271例接受I-O联合化疗患者,814例(19%)为鳞癌,3457例(81%)为非鳞癌。可评估PD-L1水平患者中,PD-L1<1%, 1%–49 %, 和50 %–100 % 的患者分别有30%, 29 %, 和19 %。鳞癌患者的中位OS为10.6个月(95 %CI, 9.3–11.8),非鳞癌患者的中位OS为12.0个月(95 % CI, 11.3–12.8)。鳞癌和非鳞癌患者的12个月、24个月的OS率分别为45.1 % 、24.5 %和49.9 % 、32.5 %。不管组织类型,PD-L1≥50 %患者的OS较低表达患者明显延长。鳞癌和非鳞癌患者中,ECOG≥2和脑转移患者均与较差的OS有关。
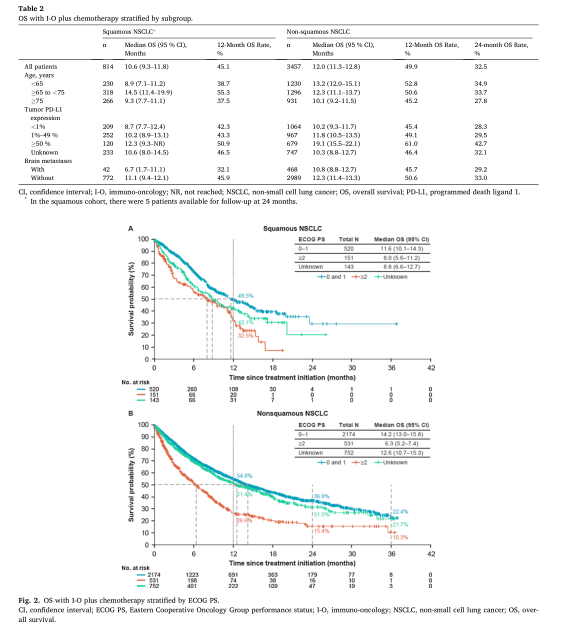
I-O联合化疗疗效评估
3041例接受单药免疫治疗患者,其中875例(29 %)为鳞癌,2,166例(71 %)为非鳞癌。可评估PD-L1水平患者中,PD-L1<1%, 1%–49 %, 和50 %–100 % 的患者分别有5%, 13 %, 和70 %。鳞癌患者的中位OS为11.3个月(95 % CI, 9.8–12.8),非鳞癌患者的中位OS为14.1个月 (95 % CI, 12.4–15.8)。鳞癌和非鳞癌患者的12个月、24个月、36个月的OS率分别为48.7 %、27.8 %、18.2 %和52.9 %, 38.5 %, 29.9 %。PD-L1≥50 %的非鳞癌患者的OS较低表达患者明显延长。鳞癌患者中脑转移中位OS较非脑转移短,但是在非鳞癌患者中无明显差别。不管组织类型,ECOG PS评分0–1患者的中位OS较ECOG PS评分≥ 2的明显延长。
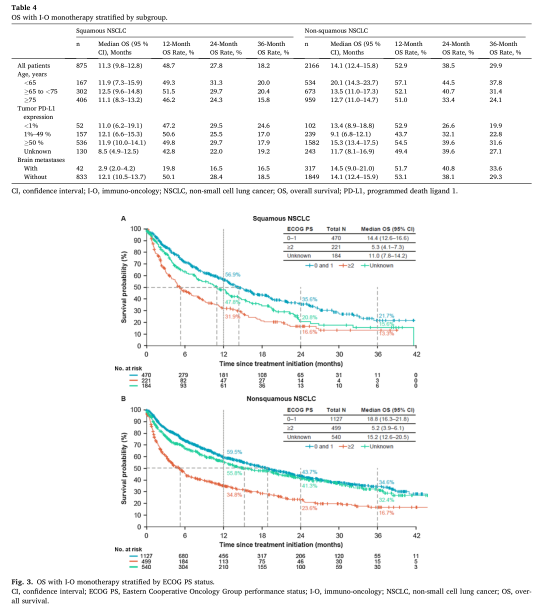
I-O单药治疗疗效评估
综上,真实世界研究评估的,免疫治疗一线治疗晚期非小细胞肺癌(NSCLC)患者的生存较临床研究的要低,表明对此需要进一步改进治疗措施。
原始出处:
Waterhouse D, Lam J, Betts KA, et al. Real-world outcomes of immunotherapy-based regimens in first-line advanced non-small cell lung cancer. Lung Cancer. 2021 Jun;156:41-49. doi: 10.1016/j.lungcan.2021.04.007. Epub 2021 Apr 14. PMID: 33894493.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#非小细胞#
34
#真实世界#
42
真实世界还是真实世界
55
谢谢梅斯提供这么好的信息,学到很多
55
NSCLC下一步突破在于新靶点了,靶向治疗和免疫治疗基本见顶了,再有新的就需要新机制了
48